What is the Gut-Brain Axis and Microbiome?
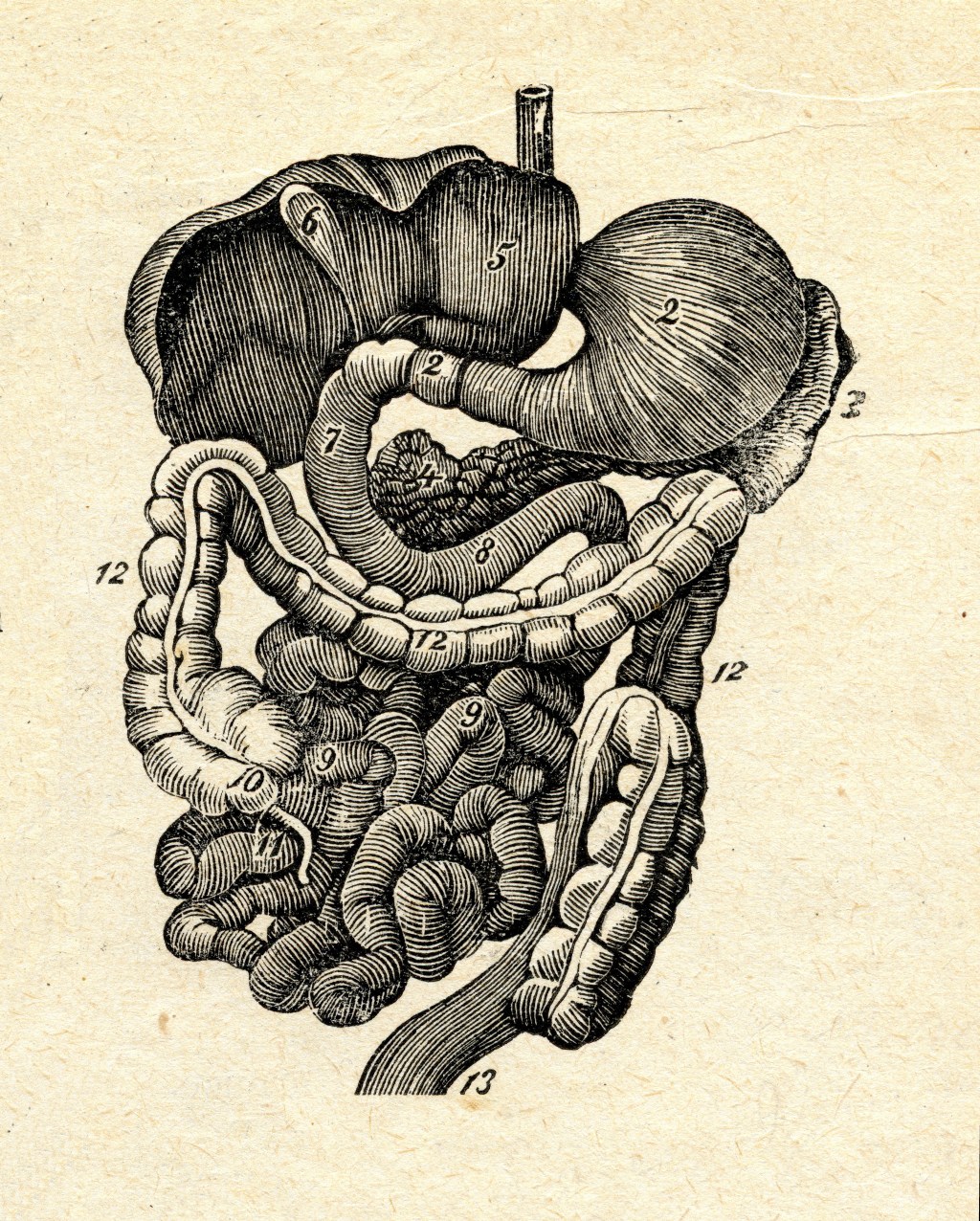
- The gut (gastro-intestinal tract) and the brain communicate across a bi-directional neural network, referred to as the gut-brain axis (informally mini-brain).
- The vagus nerve is the prominent component of the gut-brain axis.
- The microbiome refers to the trillions of microorganisms that live in and on humans.
- For every cell in our body, there is at least one bacterial cell.
- Some gut microorganisms help produce an array of neurotransmitters associated with mood, cognition and reward (e.g., serotonin, GABA, and dopamine). For example, 90% of the body’s serotonin is found in the gut.
- Other gut microorganisms make enzymes to digest food.
- Research has demonstrated the association of an imbalanced microbiome with Alcohol Use Disorders (AUDs), including the “development and progression” of AUD.
- Alcohol abuse has profound effects on the gut microbiome.
- Primarily by killing beneficial bacteria and increasing gut inflammation.
- It may take several weeks or even months to fully restore a healthy gut microbiome.
- Recent research demonstrated a significant decrease of cravings with microbiome treatments, including fecal microbiota transplantation.
- Imbalanced microbiomes have also been associated with depression, anxiety, Alzheimer’s, and Parkinson’s.
- Alcohol abuse has profound effects on the gut microbiome.
How Does the Gut Respond to Food?
- The experience with and desire for certain foods involves how the food tastes, texture, and subconscious processing of taste in our gut which signal certain neuromodulators and neurotransmitters.
- The gut communicates to the brain what we think we want and, therefore, influences our behaviors around food.
- We have sensors in our gut that send signals to our brain independent of taste (e.g. sugar).
- Ingesting sugar releases dopamine (motivation, craving, desire, reward). Dopamine stimulates appetite. That is why it is common to crave sugar after we stop drinking.
- When we ingest carbohydrates, our brain releases serotonin (happiness, focus, calm). Serotonin suppresses appetite.
- The gut also detects proteins (amino acids that are building blocks of muscle and neurochemicals). We feel full when we ingest an adequate amount of protein.
Why is Mindset Important?
- Our mindset can change our gastric (stomach) enzymes. Here is a link to a powerful study. Mind over milkshakes: mindsets, not just nutrients, determine ghrelin response – PubMed (nih.gov)
What are Nutrition Basics for Gut Health to Promote Health and Recovery?
- Eat at consistent times. This is also important for circadian rhythm.
- Be aware of sugar intake, especially “hidden sugars”.
- Eat a diet rich in:
- Fiber/prebiotics (difficult to digest complex carbohydrates known as polysaccharides that enhance the growth or activity of beneficial bacteria in the gut)
- Probiotics (live microorganisms that maintain or improve the “good” bacteria in the body)
- Support healthy gut microbiome by eating at least 1 serving of a fermented food (probiotics) per day. Probiotic supplements are also effective temporarily. Be careful not to overtake probiotic supplements.
- Eating 2 servings weekly of oily fish high in DHA and EPA omega-3 fatty acids is optimal. Taking a minimum of 1000 mg of fish oil supplement Omega-3 (EPA + DHA) can also be effective. If vegan, there are foods with AHA Omega-3 fatty acids and well as AHA Omega-3 fatty acid supplements.
- Omega-3 fatty acids are the most powerful anti-inflammatory micronutrients that we can ingest.
- In addition to multiple physical health benefits, it can improve mood (independently decrease mild depression and anxiety and even enhance effectiveness of antidepressants) and decrease pain.
- Note EPA Omega-3 fatty acids appear to be the best in fighting depression and anxiety.
- Change mindset from “diet” to “nutrition plan” …
Gut-Brain Axis | Psychology Today
Proposed questions for thought/sharing:
1. Have you changed when and/or what you eat, including supplements, and how have those changes supported your recovery/wellness?
2. What are your challenges to change when and/or what you eat, including supplements? Any ideas for the future?
3. How has your mindset either supported or interfered with your healthy eating?
Disclaimer:
This summary is for general informational purposes only and does not constitute the practice of medicine or other professional health care services, including the giving of medical advice, and no doctor/patient relationship is formed.

Leave a comment