This post briefly reviews a recent randomized clinical trial using a single 800 mg dose of Cannabidiol in a cohort of individuals with moderate to severe alcohol use disorder. Relevant information from preclinical animal studies is also reviewed.
Alcohol use disorder (AUD) remains a leading health problem worldwide affecting approximately 400 million people. It is a leading cause of morbidity and mortality. Despite advances in understanding of neurobiological mechanisms and risk factors for AUD treatments available are under utilized and only moderately effective.
There are three FDA approved medications to treat AUD and several others used off label. There have been reviewed in earlier posts here here, and here. There have been preclinical studies suggesting that Cannabidiol (CBD) a non psychoactive substance present in hemp and cannabis plants may decrease alcohol use and symptoms in people with AUD.
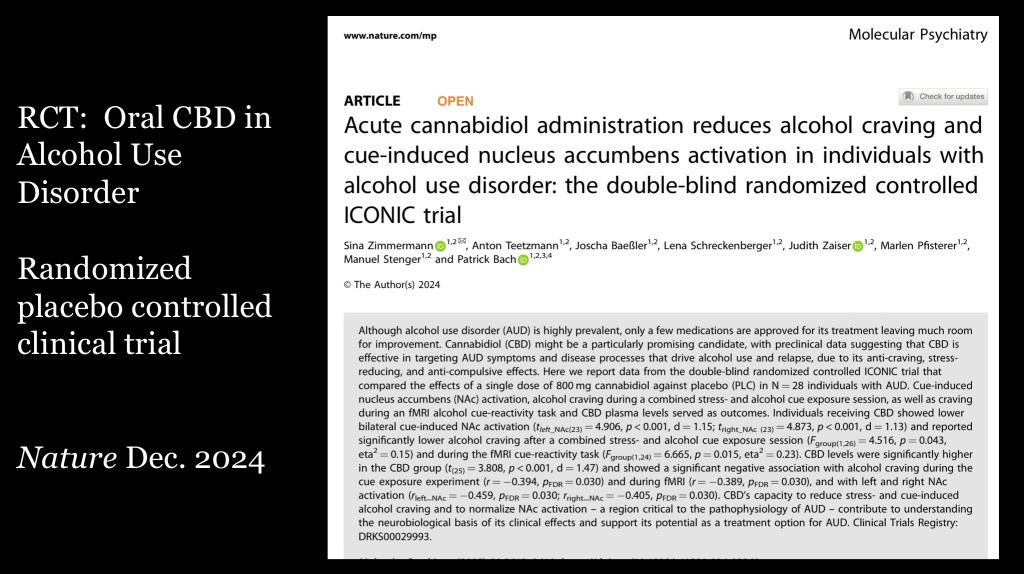
This study was published in the journal Nature; Molecular Psychiatry December 2024. It also was featured in several media reports. The study used a single large dose of oral CBD along with stress and alcohol cue stimuli. This was followed by fMRI focusing on activity in the nucleus accumbens, an area of the brain known to play a key role in mediating attention and motivational drive in alcohol and other addictions.
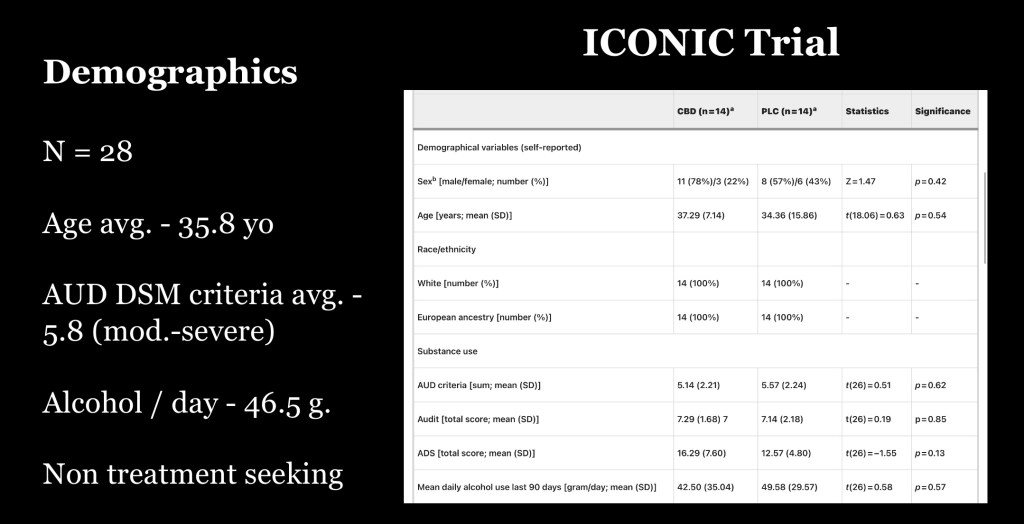
Twenty-eight subjects were included in the study and randomly assigned to either CBD or control group. The study was double blinded. All subjects met DSM-5 criteria for moderate to severe AUD and were not seeking treatment. The subjects were instructed to remain alcohol free for 24 hours prior to the study date. A single oral dose of 800mg synthetic CBD was administered.
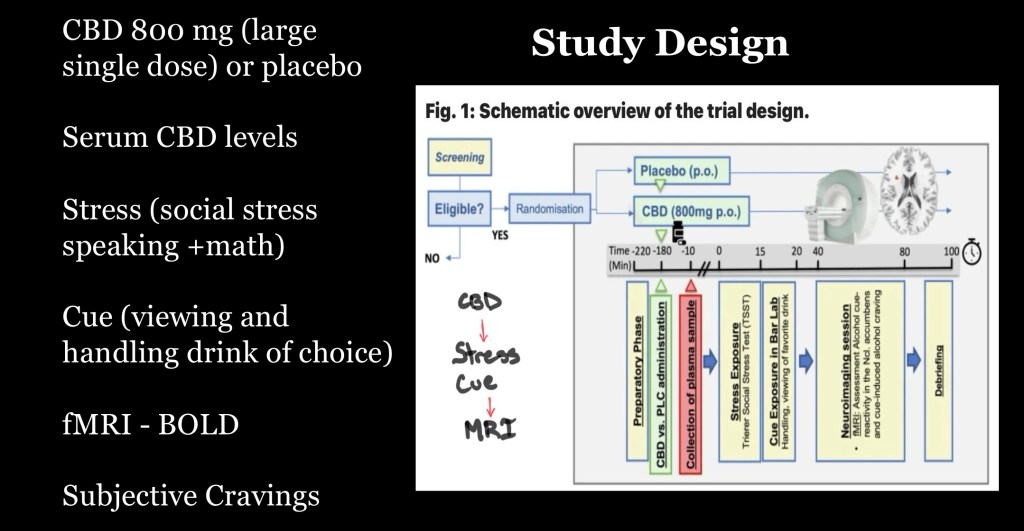
Following a waiting period to allow for peak plasma level subjects underwent stress by a social speaking and verbal math protocol (Trier test)They were then exposed to alcohol cues in a “lab bar” setting by viewing and directly handling bottles of alcohol beverage of choice.
Immediately following cue exposure the participants underwent structural and fMRI-BOLD imaging. In a separate test subjects were shown alcohol or neutral visual cues while in the MRI scanner and fMRI sequences were obtained. Subjective craving scores were also obtained during the study.
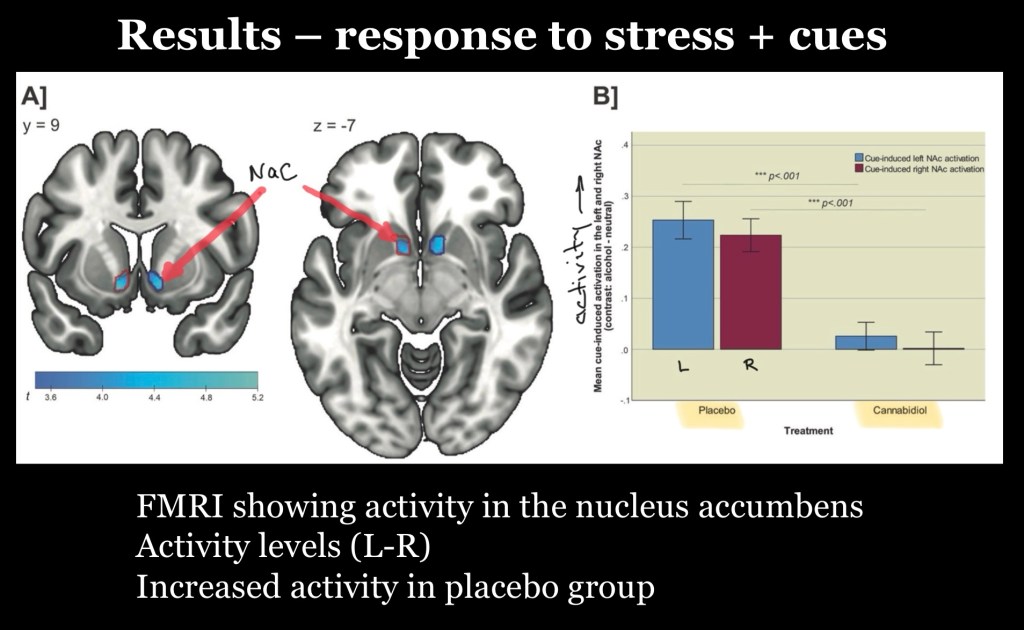
Test results are shown above. Raw data was post processed and subtracted to demonstrate signal changes under test conditions (alcohol cue-neutral). Blue areas in the MRI images represent activity in the Nucleus Accumbens (NaC). The bar graphs show marked elevation in activity in placebo subjects compared to CBD subjects. This indicates physiologic suppression of combined stress and alcohol cues by CBD.
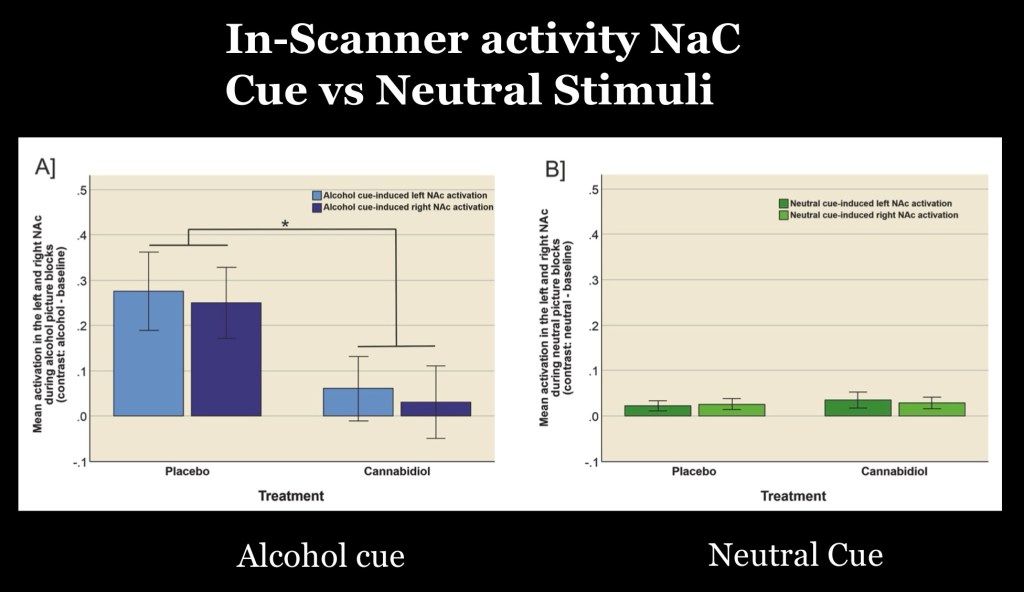
NaC activity due to alcohol related pictures during the scan on the left demonstrate marked increased activity in placebo subjects. Activity in the NaC was suppressed by CBD.
The graph on the right shows minimal activity in both groups with neutral cues. This suggests specific alcohol related sensitivity response in persons with AUD. This activation is suppressed by CBD.
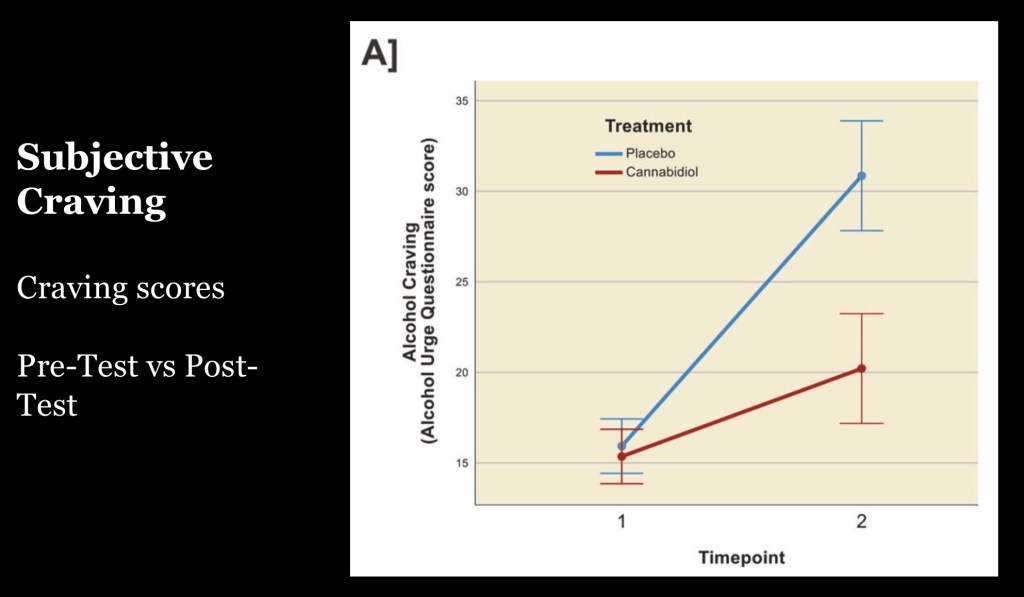
Data showing active subjective craving rating during the MRI imaging phase, Decreased overall intensity of cravings found in CBD group.
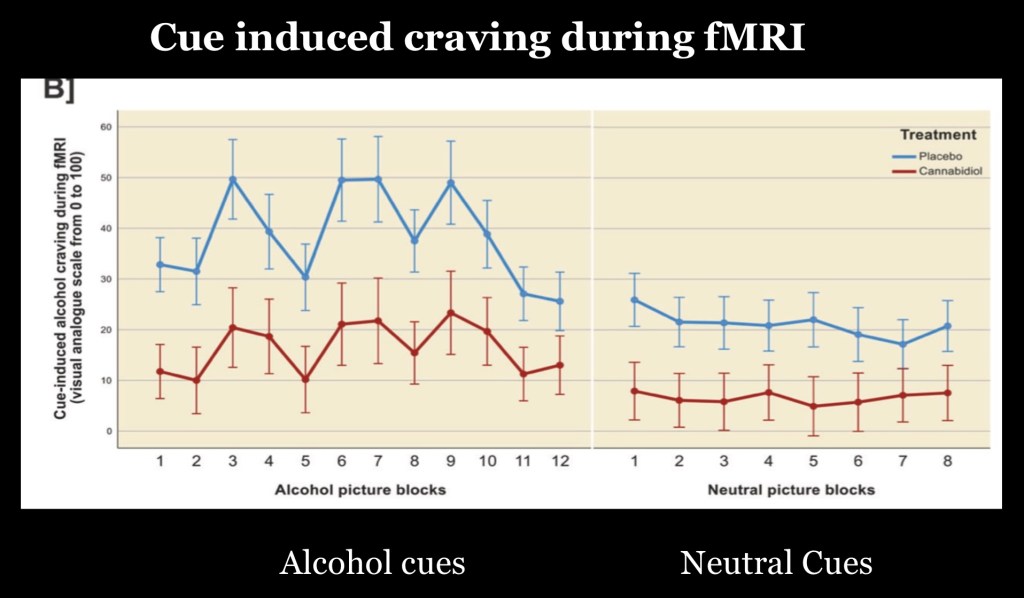
Craving scores in the in-scanner experiment demonstrating blunted response to alcohol cues in the CBD group.
The next section reviews some of the supporting evidence obtained from preclinical studies on CBD effects in chronic alcohol use.
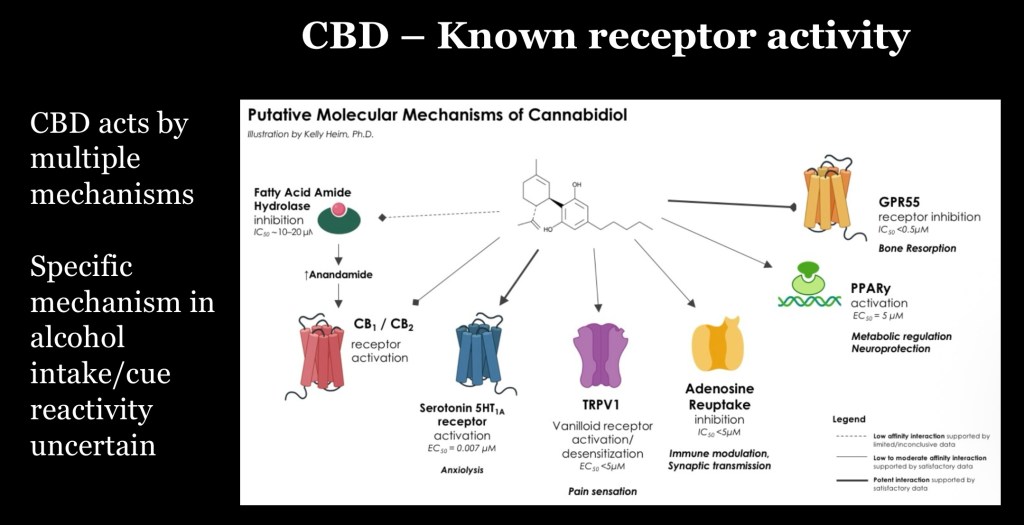
The cannabis plant contains over 100 phytobiological cannabinoids. CBD was first isolated in 1940, however it is not psychoactive and was thought to be inert in humans. It was largely ignored in research until recently. It only interacts weakly with the endocannabinoid receptors CB1 and CB2 acting as a reverse agonist.
The above diagram summarizes known receptors interacting with CBD. The mechanism responsible for therapeutic effects in AUD is unknown at this time.
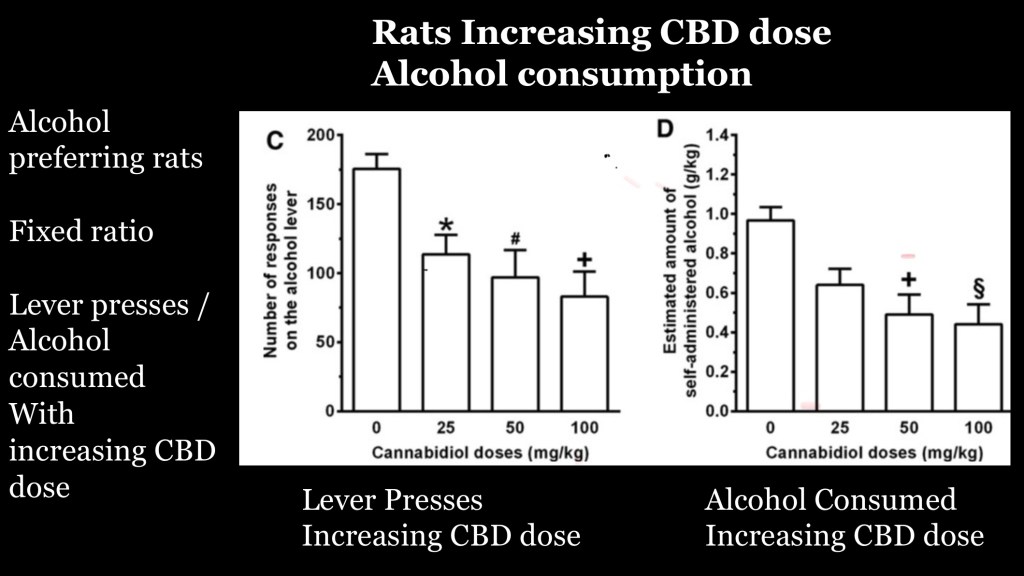
This study looked at the effects of CBD in alcohol preferring rats. The study used increasing doses of injected CBD in rats conditioned to receiving alcohol by lever presses in a fixed reinforcement schedule.
The chart on the left reflects number of lever presses. The graph on the right reflects alcohol dose received per session. Results demonstrate a clear dose-response relationship consistent with pharmacological effect on drug seeking behavior.
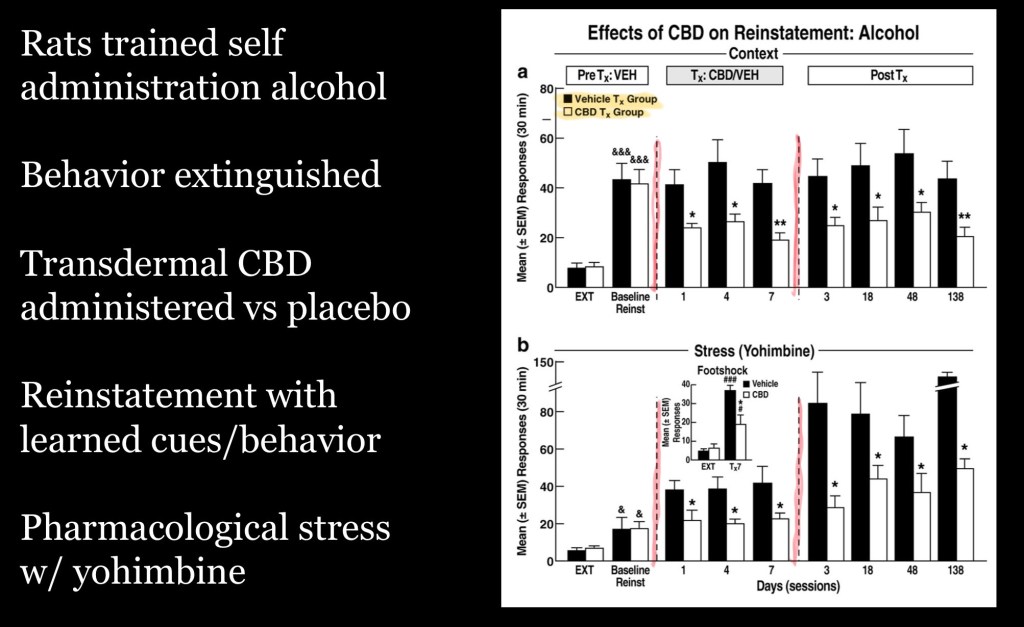
This study examined the effects of CBD in rats following conditioning and extinction of alcohol seeking behavior.
Black bars = controls
White bars = CBD group
The top graph is divided into three phases:
The first stage represents alcohol seeking (nose poke) prior to treatment. Responses are equal
Second stage represents responses following extinction with CBD/placebo. CBD group has fewer alcohol seeking behaviors
Third stage after CBD discontinued up to 138 days. Continued decrease in seeking response with no active treatment.
The bottom graph represents seeking response under pharmacological stress (yohimbine administration). Again significantly fewer responses in the CBD group. Pattern continues past discontinuation of CBD treatment.
These findings expand on previous results indicating a durable response during a preclinical relapse model present even under stressful conditions.
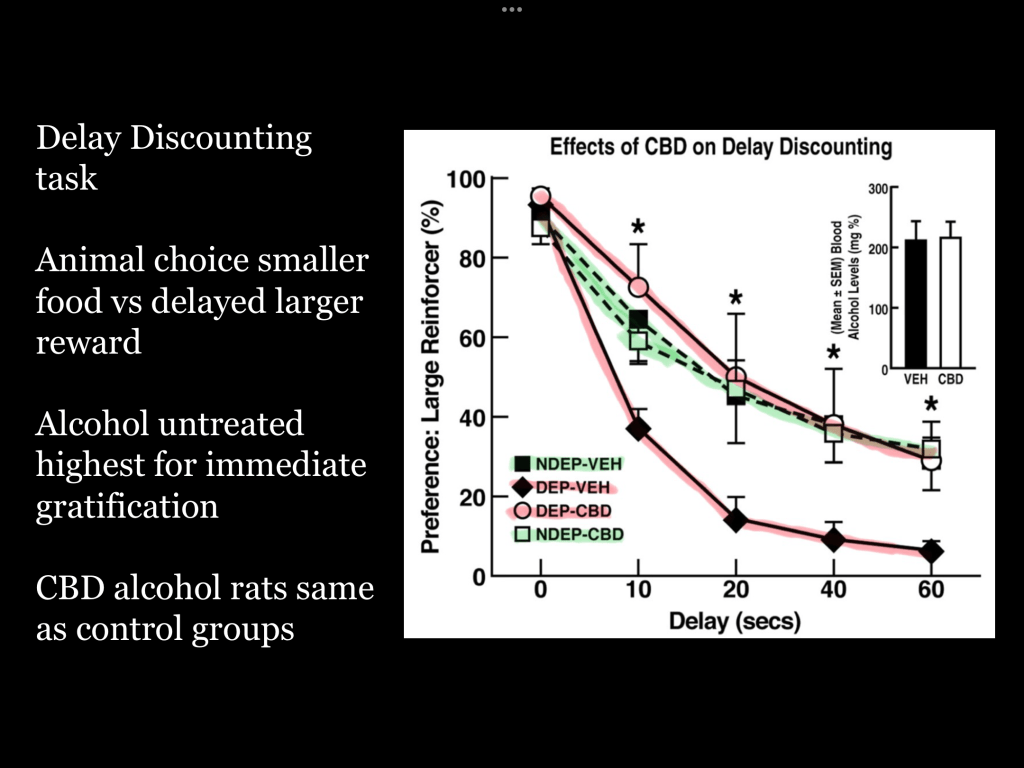
Delay discounting refers to the tendency to prefer smaller immediate rewards over larger future rewards. It is an indirect marker of impulsivity and has a strong association with addiction.
Alcohol dependent groups are colored in red. Nondependent rats in green. The graph demonstrates that only non treated alcohol dependent rats had increased preference for immediate rewards over delayed larger rewards. CBD treated dependent rats were identical in response to controls. Improved impulse control is likely to improve clinical outcomes in AUD.
Several important limitations in this study should be pointed out. It was not designed to test for direct clinical application of CBD in treatment of alcohol dependance. This was a small scale study building on preclinical animal evidence. The aim was to test a single dose in individuals with AUD and correlate that with the neurological mechanism of activation in the nucleus accumbens. Secondarily short term reduction in cue induced craving was also assessed. This supports the need for additional clinical trials evaluating treatment paradigms over longer term and in non laboratory settings.
…………………………………………………………………………
Small numbers of subjects may over or underestimate measured effects. Limitations inherent in MRI based studies due to cost and time constraints typically require smaller study sizes. Additionally, the larger single dose used in this study may not translate to ideal daily dose or other strategies which may be better suited to longer term treatment. The duration of effect and overall disease progression cannot be assessed by this single time point study.
It should be noted that decades of research have resulted in only one FDA approved therapeutic indication for CBD, the anti-seizure medication Epidolex. Many other promising agents found effective in preclinical studies have been proven ineffective in human trials.
Cannabidiol is a promising potential therapeutic agent due to high safety profile, relatively low cost and lack of narcotic or addictive properties. It may be synthesized or extracted from plant sources. There are few potential side effects or drug interactions. Thus it could be use as an adjunct to other medications or psychosocial interventions. This early human laboratory type study along with preclinical studies strongly support the need for larger clinical trials.
For information and educational purposes only. This post should not be considered medical or professional advice. Images and references obtained from sources freely available on the World Wide Web.
Thank you for your time in reviewing this post. Comments and feedback are welcome. Jeffk072261@gmail.com
JK 8/25
REFERENCES
Acute cannabidiol administration reduces alcohol craving and cue-induced nucleus accumbens activation in individuals with alcohol use disorder: the double-blind randomized controlled ICONIC trial – Molecular Psychiatry
Molecular Psychiatry (2025) 30:2612–2619; https://doi.org/10.1038/s41380-024-02869-y
https://www.nature.com/articles/s41380-024-02869-y
…………………………………………….
CBD
https://www.nature.com/articles/s41380-024-02869-y
Effects of cannabidiol plus naltrexone on motivation and ethanol consumption
Adrián Viudez-Martínez, María S García-Gutiérrez, Ana Isabel Fraguas-Sánchez, Ana Isabel Torres-Suárez, Jorge Manzanares
First published: 02 June 2018 https://doi.org/10.1111/bph.14380
British Journal of Pharmacology: Volume 175, Issue 16
https://bpspubs.onlinelibrary.wiley.com/toc/14765381/2018/175/16
Functional neuroimaging studies of alcohol cue reactivity: A
quantitative meta-analysis and systematic review
Joseph P. Schacht, Raymond F. Anton1, and Hugh Myrick1,2
1Center for Drug and Alcohol Programs, Department of Psychiatry and Behavioral Sciences,
Medical University of South Carolina, Charleston, SC
Addict Biol . 2013 January ; 18(1): 121–133. doi:10.1111/j.1369-1600.2012.00464.x.
Reducing Effect of Cannabidiol on Alcohol
Self-Administration in Sardinian Alcohol-Preferring Rats
Paola Maccioni,1 Jessica Bratzu,1 Mauro A.M. Carai
Cannabis and Cannabinoid Research Volume 7, Number 2, 2022 ª Mary Ann Liebert, Inc. DOI: 10.1089/can.2020.0132
https://www.liebertpub.com/doi/pdf/10.1089/can.2020.0132
Possible Receptor Mechanisms Underlying Cannabidiol Effects on Addictive-like Behaviors in Experimental Animals
by Ewa Galaj and Zheng-Xiong Xi *
Addiction Biology Unit, Molecular Targets and Medications Discovery Branch, Intramural Research Program, National Institute on Drug Abuse, Baltimore, MD 21224, USA
Int. J. Mol. Sci. 2021, 22(1), 134; https://doi.org/10.3390/ijms22010134
………………………………………………………………………
Mueller RL, Hooper JF, Ellingson JM, Olsavsky AK, Rzasa-Lynn R, Bryan AD,
Hutchison KE (2025) A
preliminary randomized trial of the safety, tolerability, and clinical effects of hemp- derived cannabidiol in alcohol use disorder.
Front. Psychiatry 16:1516351. doi: 10.3389/fpsyt.2025.1516351
https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1516351/pdf
…………………………………………………………………………….
CANNABIDIOL AS A NOVEL CANDIDATE ALCOHOL USE DISORDER PHARMACOTHERAPY: A SYSTEMATIC REVIEW
Jasmine Turna 1,2, Sabrina K Syan 2,3,4, Benicio N Frey 4,5, Brian Rush 6, Jean Costello 6, Mark Weiss 7, James MacKillop
Alcohol Clin Exp Res. Author manuscript; available in PMC: 2020 Apr 1.
Published in final edited form as: Alcohol Clin Exp Res. 2019 Feb 19;43(4):550–563. doi:
……………………………………………………………………………..
Cannabidiol: Pharmacology and Therapeutic Targets
Stevie C. Britcha, Shanna Babalonisa, Sharon L. Walsha,
aCenter on Drug and Alcohol Research, University of Kentucky, Lexington, KY 40508, USA
Psychopharmacology (Berl) . 2021 January ; 238(1): 9–28. doi:10.1007/s00213-020-05712-8.
………………………………………………………………………………
?……………………………………………………………………………
Therapeutic Prospects of Cannabidiol
for Alcohol Use Disorder and
Alcohol-Related Damages on
the Liver and the Brain
Julia De Ternay, Mickaël Naassila, Mikail Nourredine, Alexandre Louvet
Front. Pharmacol. 10:627. doi: 10.3389/fphar.2019.00627
https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00627/pdf


Leave a comment