
Psilocybin ( 4-phosphoryloxy-N,N-dimethyltryptamine) is a psychoactive substance found in over 100 species of mushrooms native to central and South America. This post reviews the known pharmacology and effects of psilocybin along with examples of clinical investigations. Potential therapeutic use in treatment of major depression, OCD, and substance use disorders has recently been the subject of renewed interest. There is a significant need for development of more effective pharmacotherapy for treatment of substance use disorder and other psychiatric conditions. The psychedelic drugs have low addictive properties and low toxicity. Preliminary evidence suggests a potential role for psilocybin in treatment of these conditions.

Artifacts have been found dating back to 2000-3000 bc depicting ritual use of mushrooms among Central American native cultures. The agents attracted little attention in the west until the late 1950s when chemist Albert Hofmann working at Sandoz pharmaceuticals in Switzerland, synthesized LSD (Lysergic acid Diathylamide) while investigating extracts of the ergot fungus.
Hofmann reportedly accidentally ingested a dose of LSD he was working on resulting in a hallucinogenic/mystical experience.
A few years later Hofmann isolated psilocybin from mushroom samples obtained from a trip to Mexico. He was then able to synthesize psilocybin and related analogues in the lab which he often tested on himself. Sandoz marketed LSD under the brand name Delysod as well as pharmaceutical psilocybin to psychiatrists as an adjunct in psychotherapy.

Through the 1960s experimental use of LSD and psilocybin continued including by Bill Wilson cofounder of Alcoholics Anonymous. Wilson suffered from depression throughout much of his life and was enthusiastic about a possible new drug to treat depression and alcoholism.
Harvard clinical psychologist Timothy Leary became an outspoken advocate of psychedelics to achieve higher states of consciousness. The drugs became more associated with the counterculture and published scientific literature was criticized for lack of appropriate methodology and reporting. Restrictive laws were passed placing Psilocybin and LSD in category 1 status in 1970 effectively ending clinical use and research. There has been renewed interest in the recent past exploring mechanism of action and potential clinical utility.

Currently psilocybin is illegal in most of the world. Red indicates illegal status. Countries in yellow indicate ambiguous or partial legality either not enforced or selectively enforced. Blue indicates legal psilocybin. Psilocybin has been decriminalized in Colorado and Oregon as well as in some US municipalities.

The chemical structure of psilocybin is depicted above. Oral ingested dried mushrooms are most commonly used. In the body it is rapidly converted to the bio active form psilocin. Note chemical similarity to the hormone and neurotransmitter serotonin. Psilocin primarily acts on serotonin receptors.
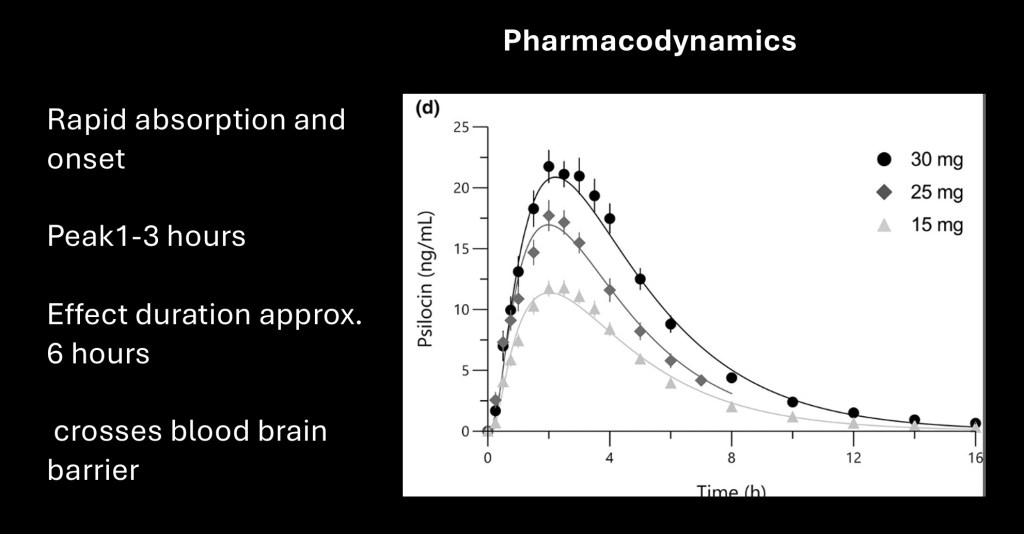
Oral psilocybin is rapidly absorbed in the GI tract. Peak effect is at 2-3 hours with duration of about 6 hours. There is considerable individual variation in response. Psylocin can cross the blood-brain barrier with resulting CNS effects, Typical oral dose is 10-25 mg. Overdose toxicity is rare and would require kilogram amounts.

Psylocybin primarily acts on serotonin receptors. There are twelve known serotonin (5-hydroxytriptamine, 5HT) receptors. Serotonin is found throughout the body including the GI tract and brain. It has diverse functions depending on the tissue and receptor type involved. Psilocybin primarily acts on the 5-HT2a receptor as a partial agonist. This is the same site of activity as LSD. It also binds to 5-HT2c and 5-HT1a receptors in the CNS.

Serotonergic pathways originate from nuclei in the brain stem and midbrain synapsing throughout cortical, cerebellar, and deeper structures. It has a role in diverse behaviors including social, emotional, motor, memory, and learning functions.
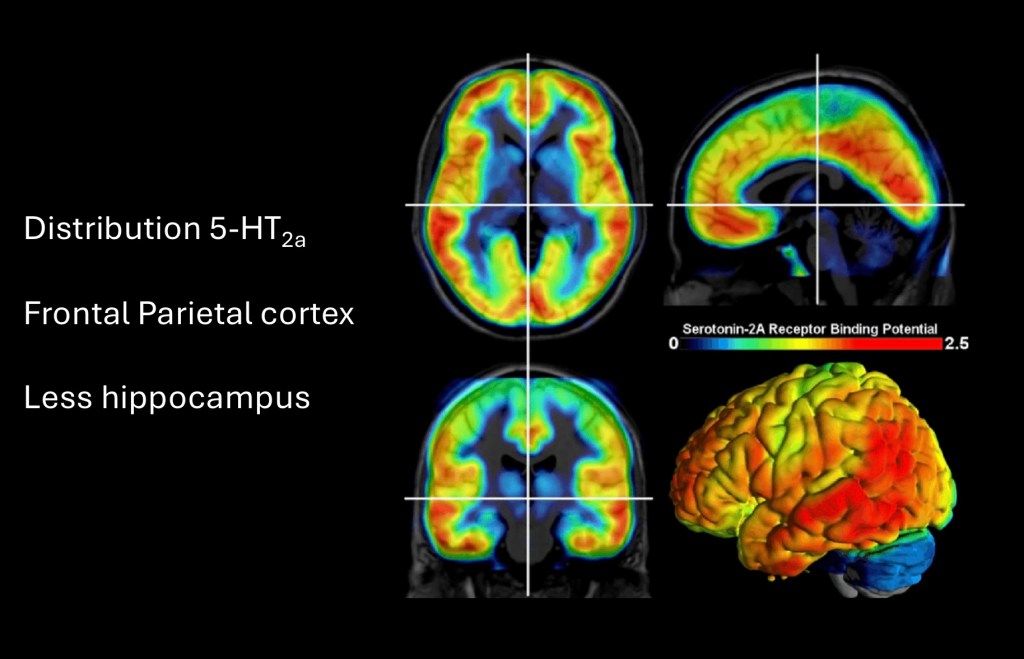
PET demonstrating distribution of 5-HT2a receptors. These are present primarily in a cortical distribution greatest in the frontal and temporal cerebral cortex. These receptors are also present to a lesser extent within the limbic system.
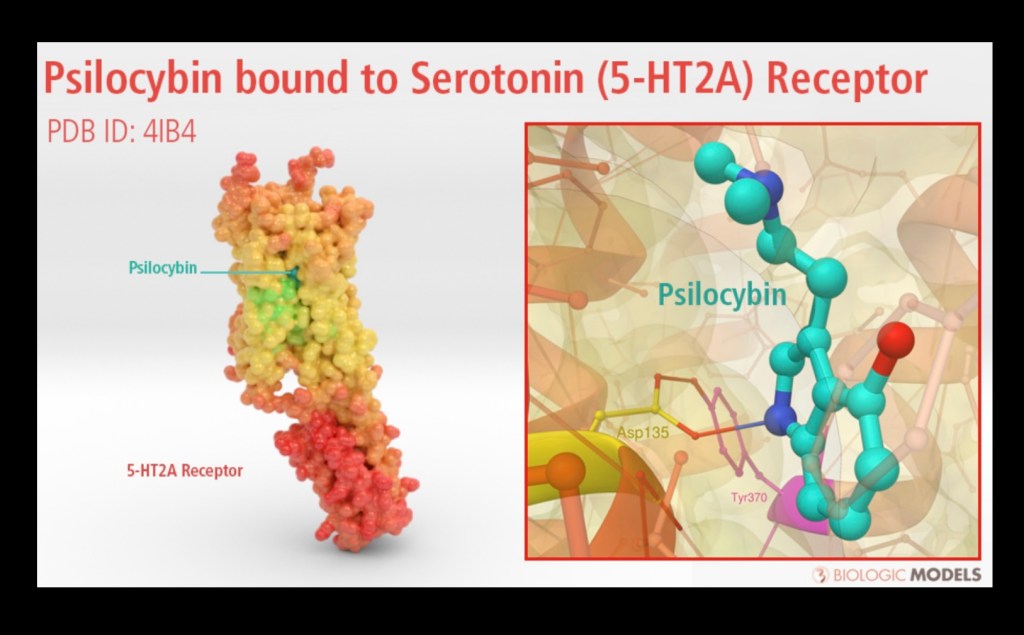
3D model depicting binding site of psilocybin. Once activated the receptor undergoes a chemical structural change. This will result in a cascade of reactions within the cell.

HT2a is a g-protein coupled receptor. These are common in plants and animals and there are over 800 known variants of g-proteins. The receptor bridges the cell membrane. Inside the cell it is bound to the g-protein which consists of three subunits. When activated the alpha subunit detaches and initiates activity within the cell. In this example adenyl cyclase activity is inhibited resulting in downstream cellular messaging.
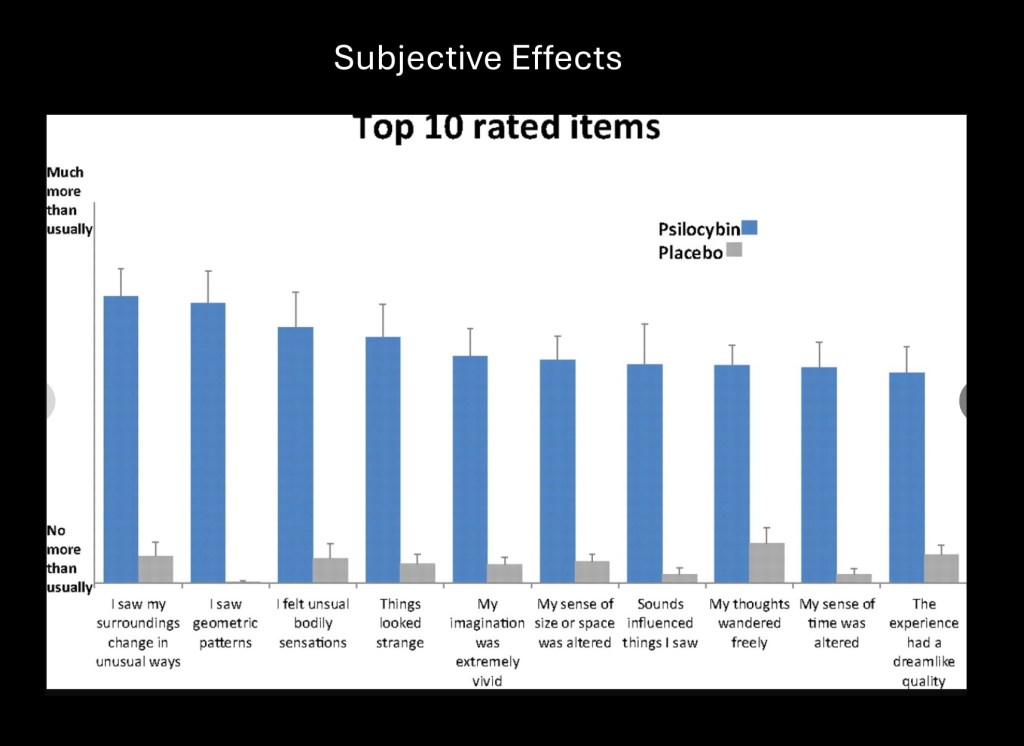
The precise cellular mechanism resulting in subjective hallucinogenic effects is not known. Altered visual perception is prominent such as distortion of objects or seeing geometric patterns. Altered sense of space and time is a frequent component. While most users describe the experience as positive, dysphoria and disturbing thoughts may also occur.

This study looked at dynamic sequential functional MRI occuring in subjects under influence of psylocybin. Altered connectivity between foci involving default and executive mode networks was identified. The lowermost row reflects net increased and decreased connectivity following psylocybin when compared with placebo.

fMRI connectivity maps following psylocybin ingestion. Extensive altered decreased connectivity within and between major neural networks was observed. These mapped to individual nodes across networks with loss of segregation and functional connectivity. The net effect is desynchronization of brain structures normally functioning in concert. Findings in similar studies suggests that desynchronization and decreased connectivity is the primary action of psychedelic drugs. It is thought that these changes may allow for neuroplastic reordering of dysfunctional pathways resulting in improvement in depression and other disease states.

This is a small nine subject open label study on effects of psylocybin in a population of individuals with alcohol use disorder. All subjects received psychotherapy along with psylocybin at weeks 4 and 8. Subjects were followed up to 36 weeks. Data above demonstrates significant decrease in total alcohol consumption and heavy drinking days persisting to 36 weeks.
Study is limited by lack of a placebo control population. Because there is no substitute capable of mimicking psilocybin effects credible placebo control has been an issue in these studies.
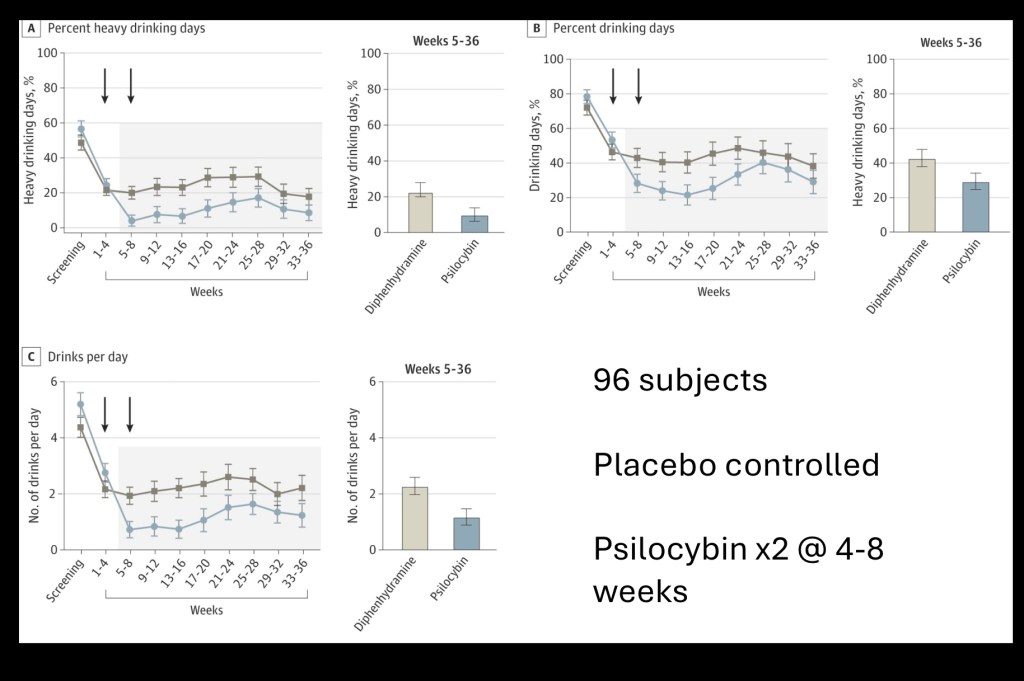
Results of a larger (n=96) placebo controlled study in alcohol use disorder. Diphenhydramine was used as placebo. All subjects received psychotherapy and a dose of either psylocybin or placebo at weeks 4 and 8.
Psylocybin subjects had fewer drinking days, decreased amount consumed, and fewer heavy drinking days compared with placebo. This demonstrates strong evidence for therapeutic benefit under controlled conditions as an adjunct to psychotherapy. Larger studies focusing on protocol, selection guidelines and risk would need to be initiated. Psilocybin, LSD and other psychedelics are schedule 1 drugs meaning high abuse potential and no medical benefit. This restricts research and medical use.
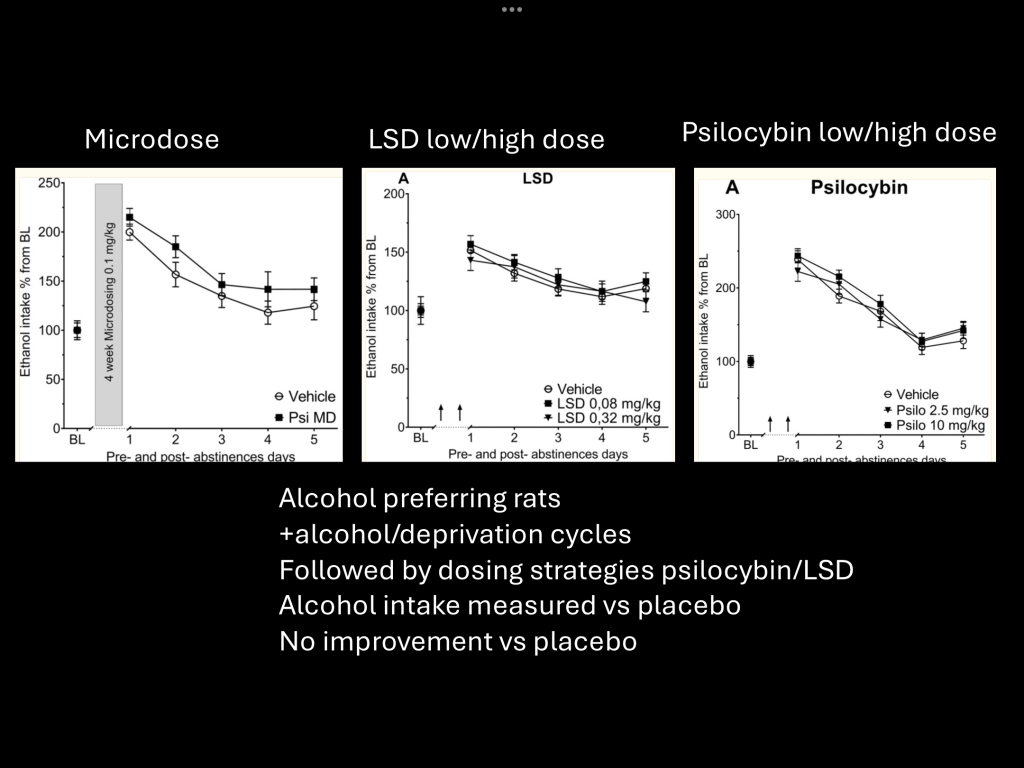
This preclinical study compared dosing strategies and psilocybin vs LSD. Rats were first given unlimited alcohol use followed by 4 deprivation/reinstatement cycles. Low vs high dose groups for both LSD and psylocybin and micro dosing of psylocybin were observed along with a placebo group.
Under these condition neither drug demonstrated benefit over placebo when animals were given unlimited access to alcohol.

MThis study looked at psylocybin in treatment resistant major depression. Nineteen subjects were included. fMRI was performed before and after Psilocybin dosing along with clinical QIDS depression scoring. Depression score with >50% reduction was considered a positive response. fMRI functional connectivity was correlated with response vs no response.
Decreased medial prefrontal cortex – hippocampus connectivity consistently predicted positive psylocybin response. This finding may serve as a predictive biomarker and provide insight into the therapeutic mechanism.

Phase two study (n=59) psylocybin was administered at start of the study and at 26 days vs daily Escitalopram (lexepro) in subjects with major depression. Double blind study was followed over 26 weeks. The red line represents the Psilocybin group. Both groups responded with decrease in depression scores. Psylocybin group demonstrated greater improvement than the Escitalopram treated subjects.
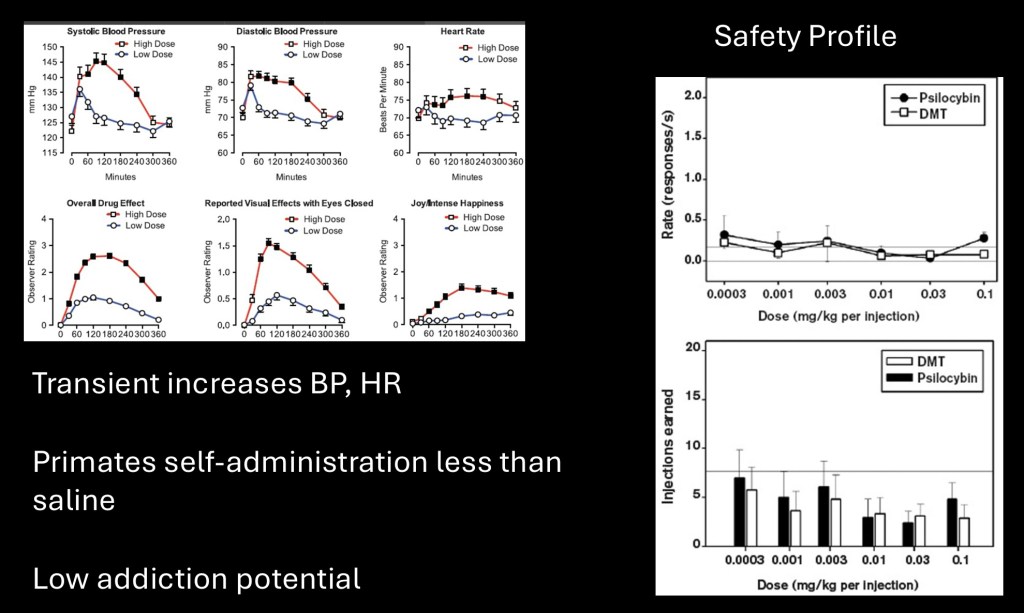
Safety profile with attention to FDA criteria. This data would be a prerequisite for potential rescheduling to category 2 or 3. High dose psilocybin resulted in transient increases in blood pressure and heart rate corresponding to dose and subjective effects. Primate studies in rhesus monkeys demonstrated no increase in self administered dose with increasing concentration of drug solutions. Addictive potential has consistently been reported as low.
………………………………………………………………..
While psylocybin has an ancient history use of the drug in western culture is fairly recent. Although illegal in most of the world cultivation of psilocybin mushrooms and illicit use is widespread. There has been a revival of scientific interest in potential use in treatment of substance use disorders, depression, OCD, and other conditions. This has prompted small scale clinical studies along with preclinical animal studies.
While early results are promising there are gaps in understanding of pharmacology and clinical limitations. Larger controlled studies may allow for FDA approval and rescheduling. At this time existing data does not seem adequate to allow for mainstream clinical use.
For information and educational purposes only. Data and images obtained from sources freely available on the World Wide Web. This post should not be considered medical or professional advice. Comments and feedback are always welcome.
References
Mushrooms
Trial of Psilocybin versus Escitalopram for Depression
Authors: Robin Carhart-Harris, Ph.D., Bruna Giribaldi, B.Sc., Rosalind Watts, D.Clin.Psy., Michelle Baker-Jones, B.A., Ashleigh Murphy-Beiner, M.Sc., Roberta Murphy, M.D.,
Published April 14, 2021 N Engl J Med 2021;384:1402-1411 DOI: 10.1056/NEJMoa2032994
Psilocybin for treating substance use disorders?
de Veen, Bas T.H. Schellekens, Arnt F.A. Verheij, Michel M.M. Homberg, Judith R.
Crossref DOI link: https://doi.org/10.1080/14737175.2016.1220834
Published Online: 2016-08-12
Published Print: 2017-02
Mhttps://doi.org/10.1080/tandf_crossmark_01
…………………………………………………………………
The abuse potential of medical psilocybin according to the 8 factors of the Controlled Substances Act
Neuro pharmacology November 2018, Pages 143-166
Matthew W. Johnson a
Roland R. Griffiths a b Peter S. Hendricks c Jack E. H
……………………………………………………….
What is the clinical evidence on psilocybin for the treatment of psychiatric disorders? A systematic review
Castro Santos, Henrique MDa,∗; Gama Marques, João MD, PhD
Porto Biomedical Journal 6(1):p e128, January/February 2021. | DOI: 10.1097/j.pbj.0000000000000128
…………………………………………………………
: Michael P. Bogenschutz MD (2016): It’s time to take psilocybin seriously as a possible treatment for substance use disorders, The American Journal of Drug and Alcohol Abuse, DOI: 10.1080/00952990.2016.1200060
………………………………………………………….
Me, myself, bye: regional alterations in glutamate and the experience of ego dissolution with psilocybin
N. L. Mason, K. P. C. Kuypers, F. Müller, J. Reckweg, D. H. Y. Tse, S. W. Toennes, N. R. P. W. Hutten, J. F. A. Jansen, P. Stiers, A. Feilding & J. G. Ramaekers
volume 45, pages 2003–2011 (2020)Cite this article
Everything we know about the 5-HT2A (serotonin) receptor
………………………………………………………………
IP3 and DAG Signaling Pathway – Mechanism, Functions, and FAQs
……………………………………………………………….
………………………………………………………….
Psilocybin desynchronizes the human brain
Joshua S. Siegel, Subha Subramanian, Demetrius Perry,
volume 632, pages 131–138 (2024
Psilocybin desynchronizes the human brain | Nature
Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms
Robin L Carhart-Harris, Leor Roseman, Mark Bolstridge, Lysia Demetriou
Scientific Reports volume 7, Article number: 13187 (2017
Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms | Scientific Reports
Rieser, Nathalie M; Herdener, Marcus; Preller, Katrin H (2022). Psychedelic-Assisted Therapy for Substance Use Disorders and Potential Mechanisms of Action. Current Topics in Behavioral Neurosciences, 56:187-211.
DOI: https://doi.org/10.1007/7854_2021_284
………………………………………………..
August 24, 2022
Percentage of Heavy Drinking Days Following Psilocybin-Assisted Psychotherapy vs Placebo in the Treatment of Adult Patients With Alcohol Use Disorder
A Randomized Clinical Trial
JAMA Psychiatry. 2022;79(10):953-962. doi:10.1001/jamapsychiatry.2022.2096
…………………………………………………………..
Mystical Experience Questionnaire
Psilocybin-assisted treatment for alcohol dependence: A proof-of-concept study
1 1 1 Michael P Bogenschutz , Alyssa A Forcehimes , Jessica A Pommy ,
Journal of Psychopharmacology mj1–11 The Author(s) 2015
Reprints and permissions: sagepub.co.uk/journalsPermissions.nav DOI: 10.1177/0269881114565144
Long-term Follow-up of Psilocybin-facilitated Smoking
Cessation
Matthew W. Johnson, PhD1
Albert Garcia-Romeu, PhD1, and Roland R. Griffiths, PhD1,2
1Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore, MD
Am J Drug Alcohol Abuse . 2017 January ; 43(1): 55–60. doi:10.3109/00952990.2016.1170135.
August 31, 2023
Single-Dose Psilocybin Treatment for Major Depressive Disorder
A Randomized Clinical Trial
Charles L. Raison, MD1; Gerard Sanacora, MD, PhD2; Joshua Woolley, MD, PhD3,4; et al
JAMA. 2023;330(9):843-853. doi:10.1001/jama.2023.14530
DARK Classics in Chemical Neuroscience: Psilocybin
Haden A. Geiger,† Madeline G. Wurst,† and R. Nathan Daniels*,†,‡
pubs.acs.org/chemneurom
A Review of Lysergic Acid Diethylamide (LSD) in the Treatment of
Addictions: Historical Perspectives and Future Prospects
Mitchell B. Liester*
P.O. Box 302, 153 N. Washington Street, Suite 103, Monument, CO 80132, USA
……………..”…………………………………………………..
Classic and non‐classic psychedelics for substance use disorder: A review of their historic, past and current research
Fúlvio Rieli Mendes
September 2022, 100025
………………………………………………………………………..
2022 Oct; 14(10): e30214.
Published online 2022 Oct 12. doi: 10.7759/cureus.30214
PMCID: PMC9650681
PMID: 36381758
Potential Therapeutic Effects of Psilocybin: A Systematic Review
Monitoring Editor: Alexander Muacevic and John R Adler
Must Psilocybin Always “Assist Psychotherapy”?
Guy M. Goodwin, F.Med.Sci., Ekaterina Malievskaia, M.D., Gregory A. Fonzo, Ph.D., and Charles B. Nemeroff, M.D.
American Journal of Psychiatry
Use of psilocybin (“mushrooms”) among US adults: 2015–2018
Online Publication Date: 21 Jan 2021
Publication Date: 11 May 2021
Article Category: Research
……………………………………………………………………….
Psilocybin targets a common molecular mechanism
for cognitive impairment and increased craving
in alcoholism
Meinhardt et al., Sci. Adv. 7, eabh2399 (2021) 17 November 2021
Zhang G, Stackman RW Jr. The role of serotonin 5-HT2A receptors in memory and cognition. Front Pharmacol. 2015 Oct 6;6:225. doi: 10.3389/fphar.2015.00225. PMID: 26500553; PMCID: PMC4594018
Structure of a Hallucinogen-Activated Gq-Coupled 5-HT2A Serotonin Receptor
Kuglae Kim1,7 ∙ Tao Che1,6,7 ∙ Ouliana Panova2,7
Volume 182, Issue 6P1574-1588.E19September 17, 2020
………………………………
Canadian Society of Pharmacology and Therapeutics (CSPT) – Inhibitory constant (Ki)
……………………………………………………………………….
The Attentional Set Shifting Task: A Measure of Cognitive Flexibility in Mice – PMC
………………………………………………………….
Hallucinogens Recruit Specific Cortical 5-HT2A Receptor-Mediated Signaling Pathways to Affect Behavior
Javier González-Maeso1,7 ∙ Noelia V. Weisstaub3,4,5,7 ∙ Mingming Zhou4 ∙ … ∙ Qiang Zhou1 ∙ Stuart C. Sealfon1,2 stuart.sealfon@mssm.edu ∙ Jay A. Gingrich
Neuron ARTICLEVolume 53, Issue 3P439-452February 01, 2007
…………………………………………………………….
Larrea, A.; Sánchez-Sánchez, L.; Diez-Martin, E.; Elexpe, A.; Torrecilla, M.; Astigarraga, E.; Barreda-Gómez, G. Mitochondrial Metabolism in Major Depressive Disorder: From Early Diagnosis to Emerging Treatment Options. J. Clin. Med.2024,13,1727. https:// doi.org/10.3390/jcm13061727
Siegel, J.S., Subramanian, S., Perry, D. et al. Psilocybin desynchronizes the human brain. Nature 632, 131–138 (2024). https://doi.org/10.1038/s41586-024-07624-5
Psilocybin desynchronizes the human brain | Nature
LSD – Jensen 1963
…………………………………………………………………….
J Psychoactive Drugs. 2020 Apr-Jun; 52(2): 113–122.
Published online 2020 Jan 23. doi: 10.1080/02791072.2020.1718250
PMCID: PMC7282936
NIHMSID: NIHMS1556422
PMID: 31973684
Psychedelic Microdosing: Prevalence and Subjective Effects
Lindsay P. Cameron, BSc,1,* Angela Nazarian, MA,2 and David E. Olson, PhD
Psychedelic Microdosing: Prevalence and Subjective Effects – PMC
…………………………………………………
………………………………………….
2 minute neuroscience
………………………………………………..
Hallucinogens and Serotonin 5-HT2A Receptor-Mediated Signaling Pathways
Juan F. López-Giménez and Javier González-Maeso
Curr Top Behav Neurosci. 2018; 36: 45–73.
Hallucinogens and Serotonin 5-HT2A Receptor-Mediated Signaling Pathways – PMC
……………………………………………………………
G Protein Coupled Receptor – Classification, Characteristics, and FAQs
…………………………………………………………….
Psychedelic Psychiatry’s Brave New World
David Nutt,1,* David Erritzoe,1 and Robin Carhart-Harris1
1Centre for Psychedelic Research, Department of Psychiatry, Imperial College London, London W12 0NN, UK
Cell 181, April 2, 2020
Role OF 5-HT2C receptors in dyskinesia
Article · January 2016
……………………………………………………………………
Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin
Robin L. Carhart-Harris, David Erritzoe, Tim Williams, +11 , and David J. Nutt d.nutt@imperial.ac.uk
January 23, 2012 109 (6) 2138-2143
Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin | PNAS
………………………………………………………………………
……………………………………………………….
Microdosing: A Complete Guide to Microdosingp
…………………………………………………………
…………………………………………………………..
Loudermilk Ahahuasca scene
……………………………………………………………
http://www.psilosophy.info/resources/mushrooms_journal2.pdf
“Good Friday” experiment reviewed
…………………………………………………………..
Neuropsychopharmacology. 2020 Jul; 45(8): 1316–1322.
Published online 2020 May 5. doi: 10.1038/s41386-020-0694-z
PMCID: PMC7298021
PMID: 32369828
Psilocybin and LSD have no long-lasting effects in an animal model of alcohol relapse
1,2 Cansu Güngör,#1 Ivan Skorodumov,1 Lea J. Mertens,2 and Rainer Spanagel1
Psilocybin and LSD have no long-lasting effects in an animal model of alcohol relapse – PMC
…………..l……………………………………………………………….
JK 9/2024


Leave a comment