Brain Disease Model of Addiction
Updates from neurobiology
In 2016 a review article was published in the New England Journal of Medicine titled Neurobiologic Advances From the Brain Disease Model of Addiction authored by Nora Volkow MD, George Koob PhD, and Alan McLellan PhD directors of the NIDA, NIAAA, and the Treatment Research Institute.
Around the same time a number of additional articles on the NIH brain disease model were published in The Lancet, Journal of the AMA, and other leading medical and scientific journals. The articles were geared toward the medical, addiction treatment, and related science communities.
The concept of drug addiction as a disease is not a new development. It has met with skepticism due to inconclusive evidence for a Neurobiological basis, somewhat vague diagnostic criteria, and questionable clinical utility. Proponents of drug addiction as a moral or character defect, lack of willpower, personal choice, a type of learning similar to love, or an adaptation secondary to psychological conflict or trauma have emerged as vocally opposed to the disease concept.
In a widely cited article published in the AAAS journal Science in 1997 by Adam Leshner, then director of the NIDA, the brain disease model was again proposed. The more recent publications represent cumulative results of a large body of new evidence made possible by advances in neuroscience, medical imaging, analysis of neural networks using fMRI, genetics and gene expression, molecular biology, and epigenetics. More comprehensive studies in epidemiology and risk factors contributing to addiction risk have been made available.
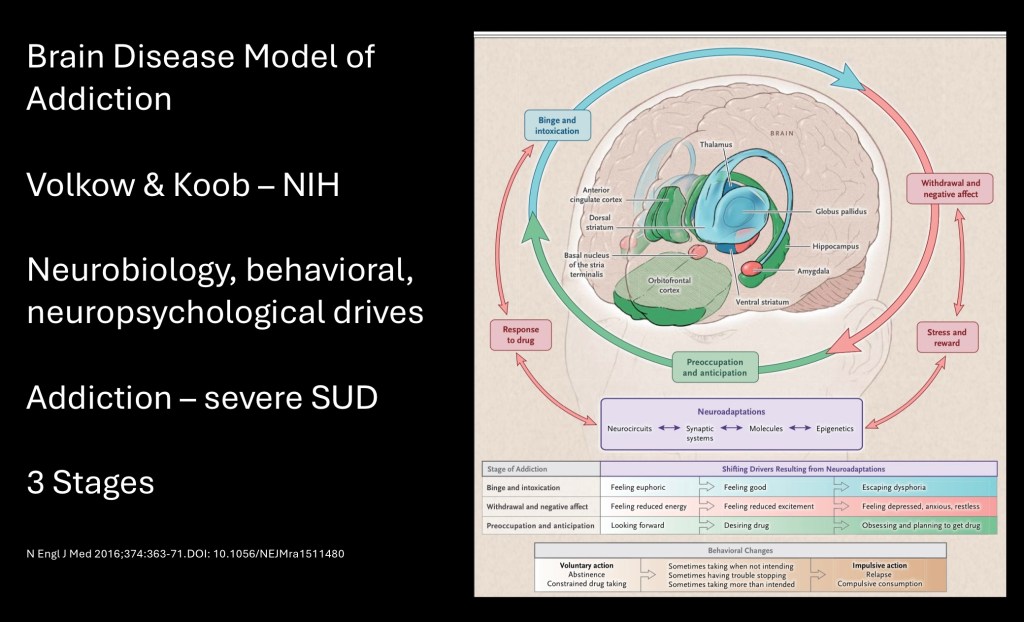
The diagram has been presented as a heuristic – a shortcut summary of a more complex body of knowledge in a clinically useful format.
The central diagram of the brain illustrates brain structures known to be pathologically altered and involved in addiction. The surrounding circle represents the addiction cycle broken down into three components, binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation. Psychological drives outside the circle include positive reward, incentive, salience, stress and negative reward. Note two way arrows connecting these elements. At the base neuroadaptations include neural circuits, synaptic systems, molecules, and epigenetics. All of these processes are dynamic and ongoing in active addiction.
Before a closer look at this model several terms should be clarified, these are what is meant by a scientific Theory and by a clinical Disease.
A theory in science has a different meaning than in common usage. A theory is an explanation of something, or a set of things observed in the world. A theory should be supported by evidence preferably multiple lines of evidence. Importantly a theory should be testable and hence falsifiable. As new evidence becomes available a theory may be replaced or updated.
Disease is meant here in the clinical sense. There is no agreed upon definition of disease. A disease consists of a harmful condition resulting in disruption of normal function of an organism. In this basic use it is difficult to exclude drug addiction as a disease similar to other diseases accepted without question.
A disease should have characteristic signs and symptoms. It should have definable diagnostic criteria. Causative factors may or may not be known. Chronic diseases are of longer duration as opposed to an acute condition. Diseases may become asymptomatic and may reoccur or not in a given case. Spontaneous or self directed remission does not exclude characterization as a disease as is sometimes claimed. Disease in practical clinical use is interchangeable with a disorder, syndrome, or pathology.
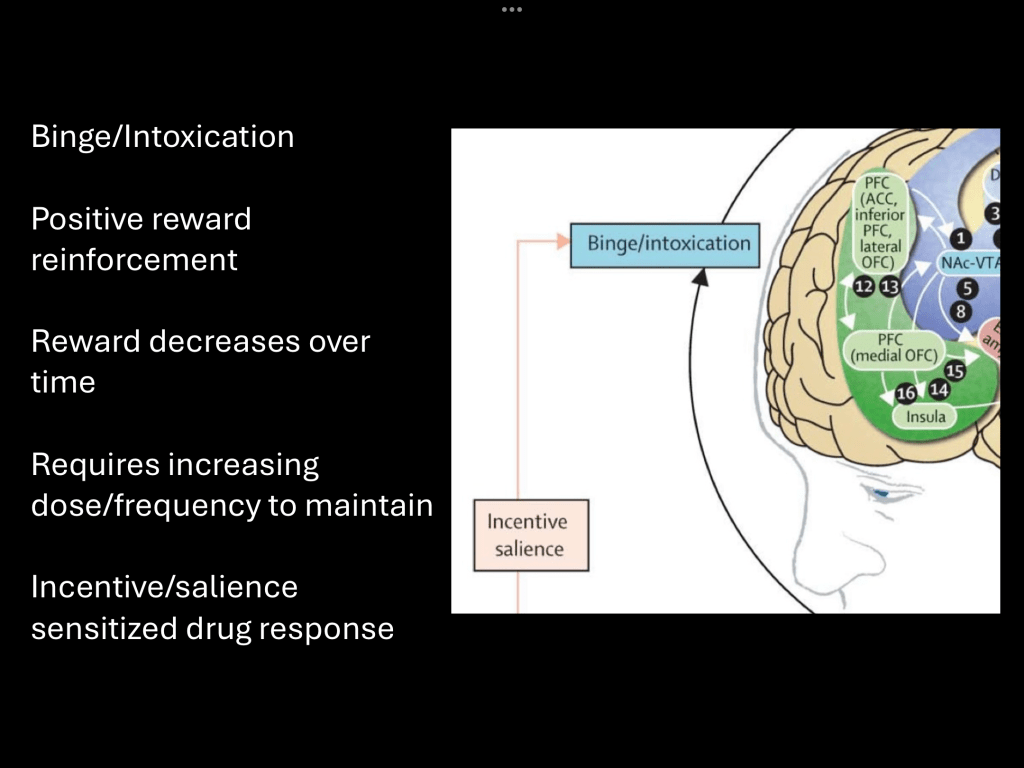
Binge/intoxication refers to the desired hedonic effect of the drug. The result is positive reinforcement of a conditioned behavior. With chronic use the drug becomes less rewarding due to tolerance and lack of novelty. There are corresponding neuroplastic changes occurring in the mesolimbic reward pathway driving disease progression.
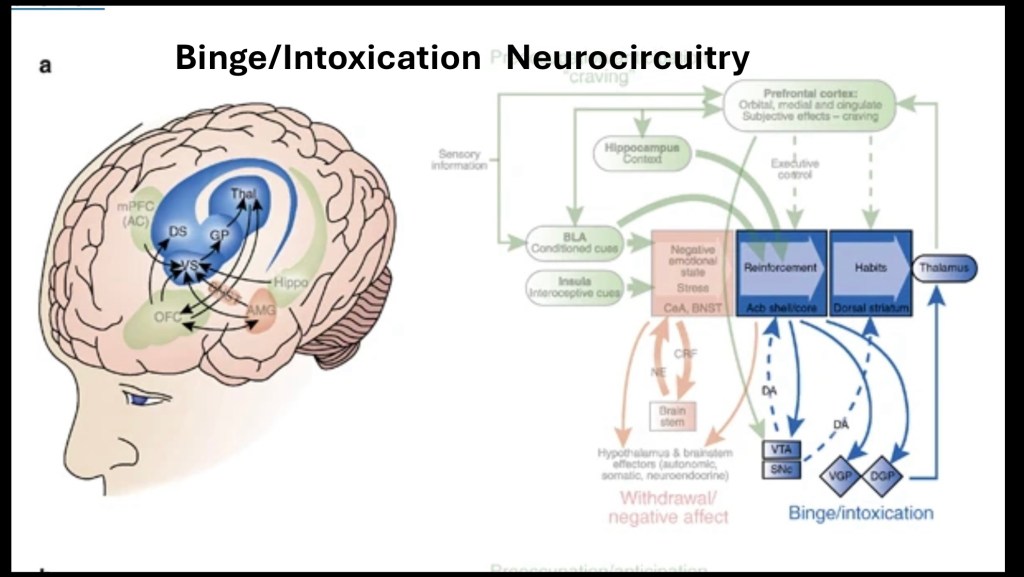
This diagram represents neurobiological changes occurring in binge/intoxication. Detailed discussion of neuroplastic mechanisms are beyond the scope of this post and are found in the references below.
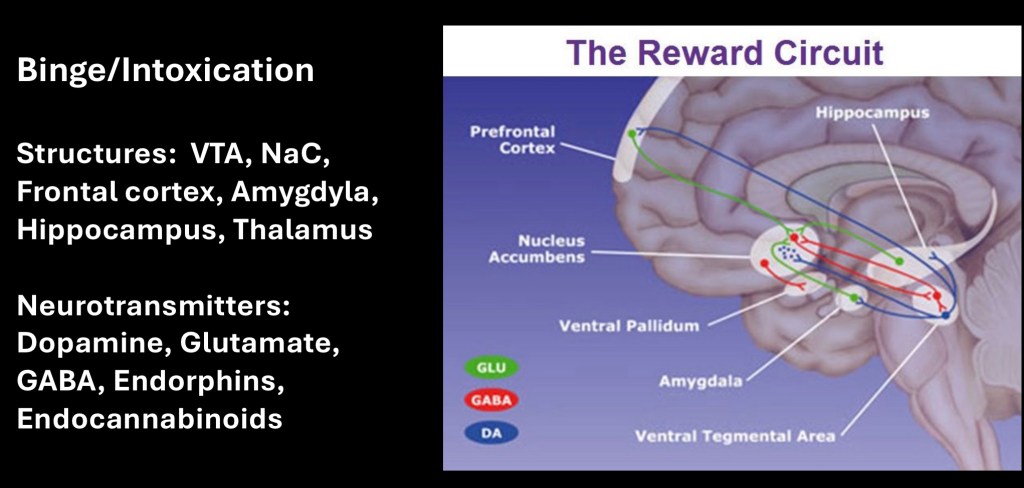
The dopaminergic mesolimbic pathway is familiar to many people concerned with addiction. The system involves additional activity and neurotransmitters involving the frontal cortex, amygdala, and hippocampus. With chronic use imbalance occurs in the reward system involving dopamine, excitatory and inhibitory signals along with endorphin and endocannabinoid modulation. Interneurons in the nucleus accumbens become sensitized to drug cues resulting in a strong motivational signal. At the same time non drug related rewards become weakened as the individual becomes narrowly focused on the addictive substance. These changes can persist into abstinence.
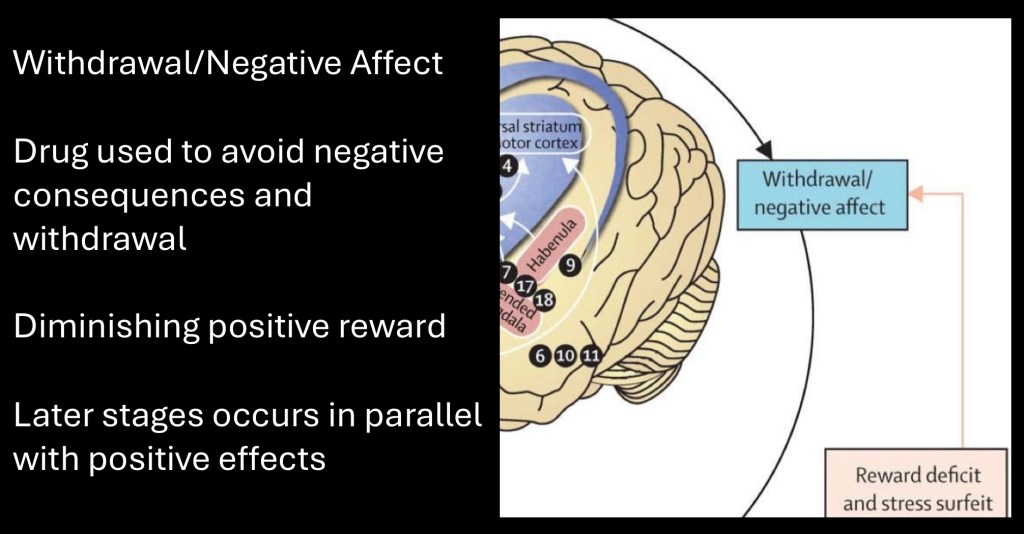
Withdrawal/negative affect increases in intensity as the addiction cycle continues. This process further reinforces the addiction as more of the substance is consumed to temporarily relieve negative feelings and emotions. The mechanism has been described as opponent – process theory.
Eventually effects exceed physiological limits and baseline affect drops lower as use continues driven almost entirely by negative consequences. This is a property found in addictive drugs not present in natural reward where the response would be to decrease or discontinue the activity.
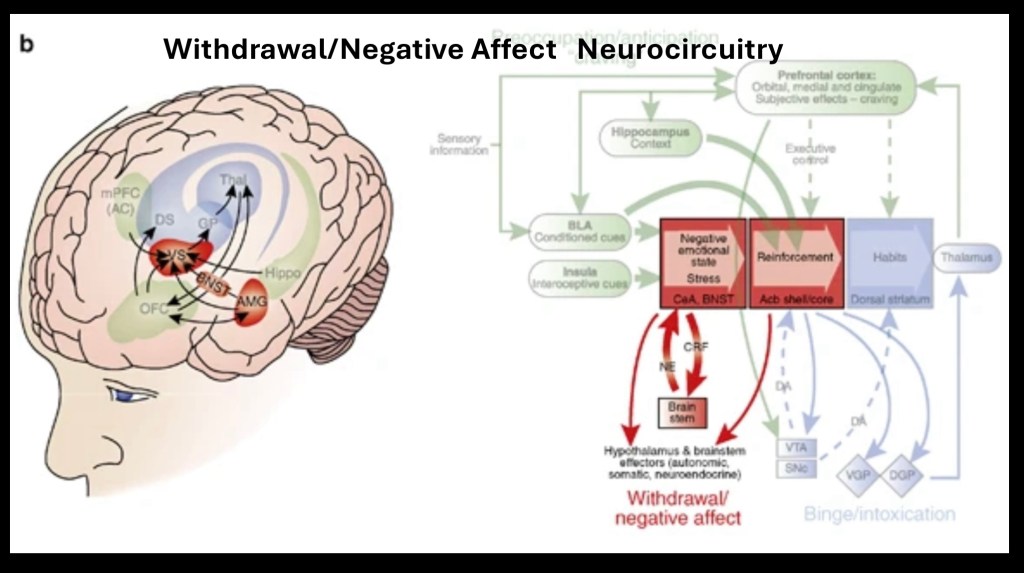
Detailed description of circuits involved and neuropathology in negative rewards corresponding to behavior are beyond the scope of this post and may be found in the references
below.
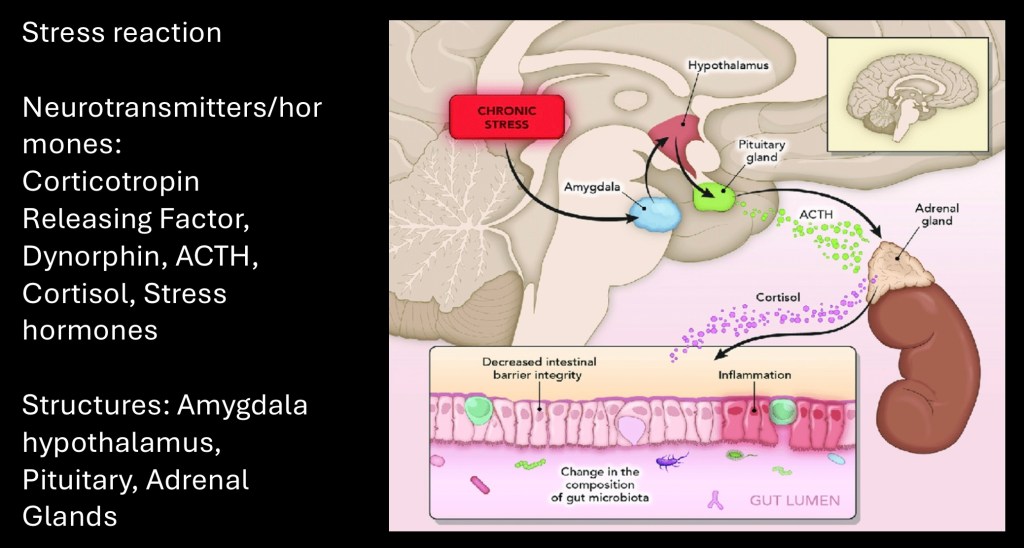
Addictive drugs with chronic use result in activation of the stress response. Intracranial structures involved are the hypothalamus and amygdala. Corticotropin releasing factor release activates the pituitary gland resulting in a systemic stress response. Epinephrine, norepinephrine ACTH, dynorphin, and cortisol hormones are generated.
This reaction normally occurs in response to natural real or perceived threats as a survival mechanism. Addictive drugs hijack this mechanism. This creates a motivational drive to consume more drug bringing temporary relief. Over time negative rewards dominate the addictive cycle.
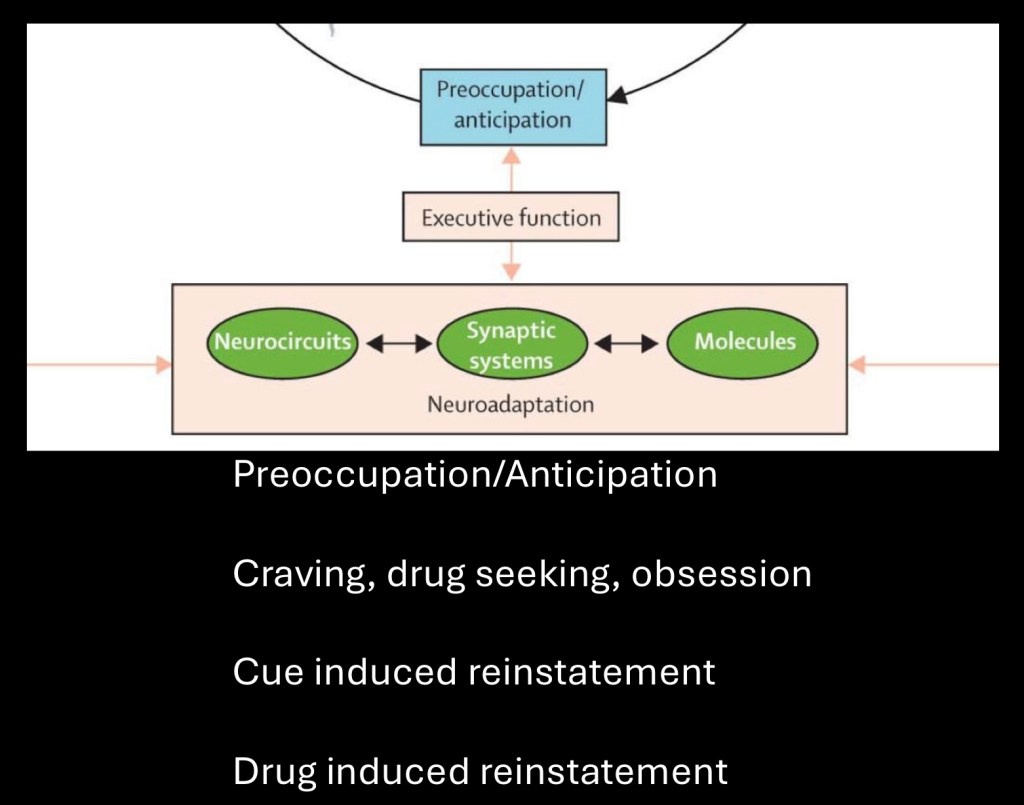
The preoccupation/anticipation phase involves executive function, subjective feelings of drug cravings, and a pattern of reinstatement following attempts at moderation or abstinence.
Neuroadaptive changes occur throughout the addictive cycle. Some of these can be long term and persist well into abstinence. Once established cellular signaling pathways become encoded into memory. Because of these changes recurrence of use tends to quickly revert to preestablished patterns.
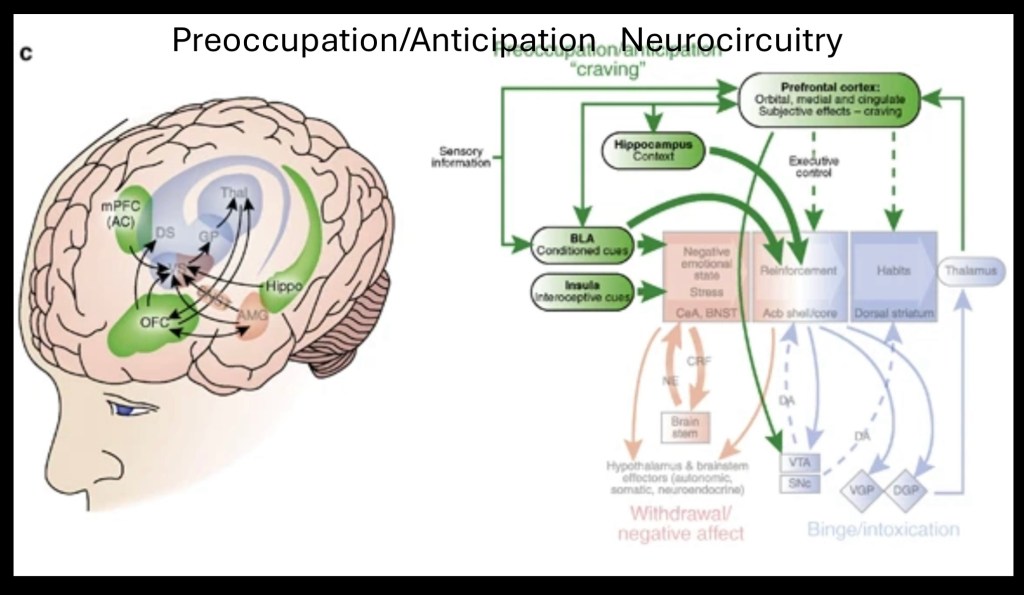
Detailed review of neural pathways is beyond the scope of this post and may be found in references below. These include sensory inputs from environmental cues, impaired executive function and decision making ability.
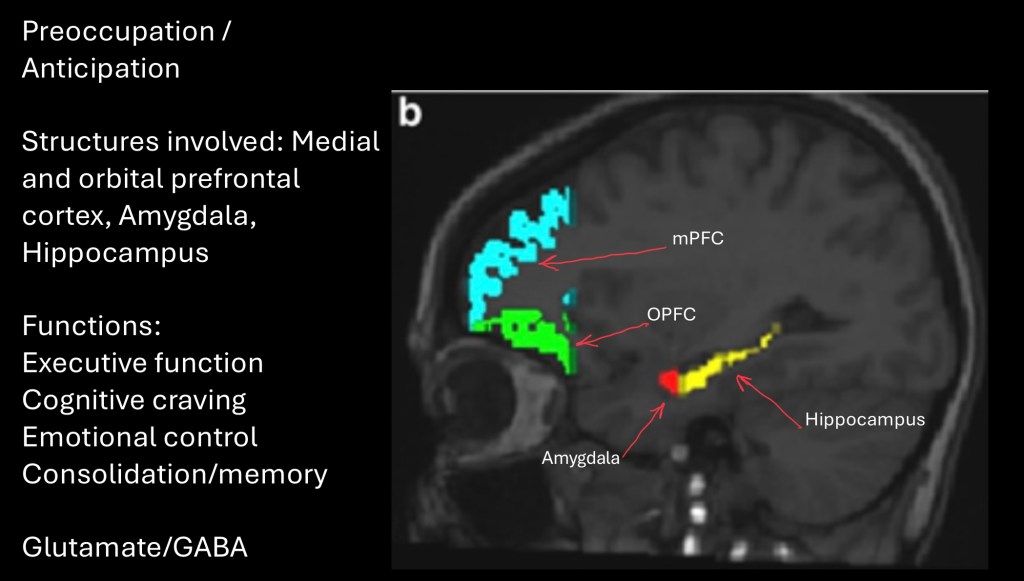
fMRI demonstrating areas of the brain affected in this phase of the addictive cycle. Frontal lobe cognitive processing, the amygdala which is key in emotional regulation, and the hippocampus involved in memory are affected. Excitatory glutamate and inhibitory GABA neurotransmitters are primarily involved.
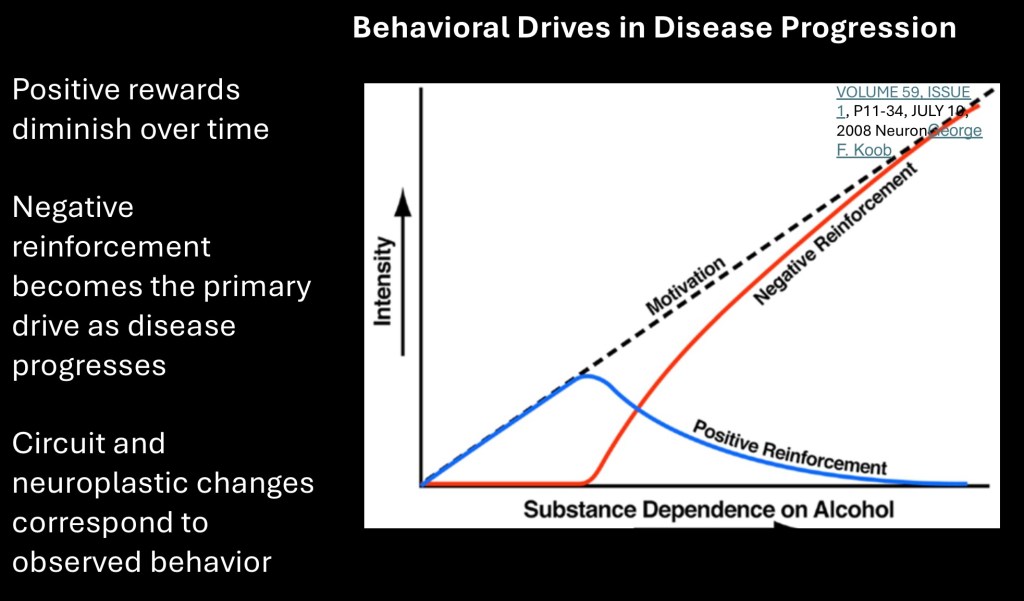
Conceptual graph showing progressive changes in intensity of positive and negative reinforcement occuring as the disease progresses. Eventually negative reinforcement where the substance is used to primarily attenuate negative consequences and maintain function dominates.
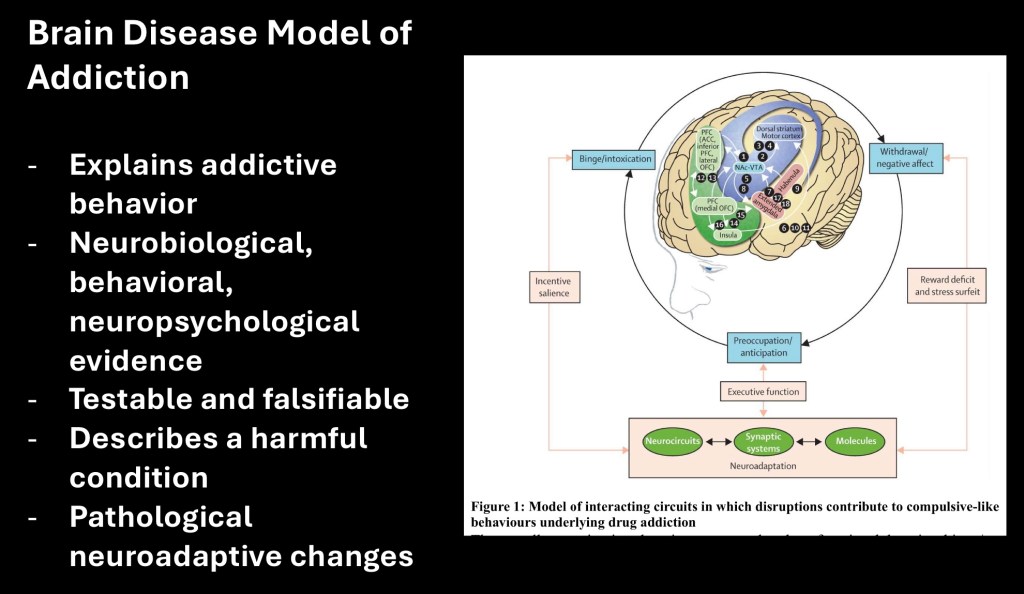
The NIH brain disease model is not intended as a comprehensive theory of substance use disorder. Root causes and risk factors are not included in this model. Specific treatment options are also not included. These aspects are discussed elsewhere.
What this model does is describe in a concise summary of the neurobiology and correlated behavioral aspects of active addiction as it progresses to the compulsive stage. We can now match observed behavior to physical abnormalities occurring in the central nervous system. The findings fit within the clinical definition of disease and definitions of a valid scientific theory.
Thank you for your consideration in reviewing this post. Data and images obtained from sources freely available on the World Wide Web. This post should not be considered medical or professional advice. Comments and feedback are welcome jeffk072261@gmail.com
References
Brain disease
The brain disease model of addiction: is it supported by the evidence and has it delivered on its
promises?
Wayne Hall, Adrian Carter, Cynthia Forli
Lancet
Psychiatry 2 105-10. 10.1016/S2215-0366(14)00126-6
……..”…………………………………………………….
Brain Disease Model of Addiction: why is it so controversial?
Nora D. Volkow, MD [Office of Director] and George Koob [Office of Director] National Institute on Drug Abuse, Bethesda, MD, 20892 National Institute on Alcohol Abuse and Alcoholism, Bethesda, MD, 20892
Lancet Psychiatry. 2015 August ; 2(8): 677–679. doi:10.1016/S2215-0366(15)00236-9.
………………………………………………………………….
Neuropsychopharmacology Reviews Published: 26 August 2009
Neurocircuitry of Addiction
George F Koob & Nora D Volkow
Neurocircuitry of Addiction | Neuropsychopharmacology
……………………………………………………………………
Leshner brain disease
…………………………………………………….
Addiction Becomes a Brain Disease
Roy A Wise
Open ArchiveDOI:https://doi.org/10.1016/S0896-6273(00)81134-4
Addiction Becomes a Brain Disease: Neuron
……………………………………………………
Addiction Becomes a Brain Disease: Neuron
Nora Volkow
……………………………………………………….
The addicted human brain: insights from imaging studies
Nora D. Volkow,1,2 Joanna S. Fowler,3 and Gene-Jack Wang1
JCI – The addicted human brain: insights from imaging studies
JCI – The addicted human brain: insights from imaging studies
………………………………………………………………
A Role for Brain Stress Systems in Addiction
George F. Koob
Neuron REVIEW| VOLUME 59, ISSUE 1, P11-34, JULY 10, 2008
https://www.cell.com/fulltext/S0896-6273(08)00530-8
……………………………………………………………
Popper, Karl: Philosophy of Science | Internet Encyclopedia of Philosophykm
……………………………………………………………..
Neurobiology of addiction: a neurocircuitry analysis
George F Koob and Nora D Volkow
National Institute on Alcohol Abuse and Alcoholism (G F Koob PhD) and National Institute on
Drug Abuse (N D Volkow MD), National Institutes of Health, Rockville, MD, USA
Lancet Psychiatry . 2016 August ; 3(8): 760–773. doi:10.1016/S2215-0366(16)00104-8.
Addiction is a reward deficit and stress surfeit disorder
Committee on the Neurobiology of Addictive Disorders, The Scripps Research Institute, La Jolla, CA, USA
Front. Psychiatry, 31 July 2013
Sec. Addictive Disorders
Volume 4 – 2013 | https://doi.org/10.3389/fpsyt.2013.00072
Frontiers | Addiction is a Reward Deficit and Stress Surfeit Disorder
Neurobiologic Advances from the Brain
Disease Model of Addiction
Nora D. Volkow, M.D., George F. Koob, Ph.D., and A. Thomas McLellan, Ph.D.
N Engl J Med 2016;374:363-71.
DOI: 10.1056/NEJMra1511480
Copyright © 2016 Massachusetts Medical Society.
https://www.nejm.org/doi/pdf/10.1056/NEJMMra1511480
…………………………………………………………………
The Neuroscience of Drug Reward and Addiction
Nora D. Volkow, Michael Michaelides, and Ruben Baler
11 SEP 2019https://doi.org/10.1152/physrev.00014.2018
The Neuroscience of Drug Reward and Addiction | Physiological Reviews
Addiction as a brain disease revised: why it still matter,s, and the need for consilience
Markus Heilig, James MacKillop, Diana Martinez, Jürgen Rehm, Lorenzo Leggio & Louk J. M. J. Vanderschuren
volume 46, pages 1715–1723 (2021)Ci
Special Communication
October 4, 2000
Drug Dependence, a Chronic Medical Illness
Implications for Treatment, Insurance, and Outcomes Evaluation
A. Thomas McLellan, PhD; David C. Lewis, MD; Charles P. O’Brien, MD, PhD; et al
JAMA. 2000;284(13):1689-1695. doi:10.1001/jama.284.13.1689
(Abstract only),
………………………………………………………………..
Addiction as a brain disease revised: why it still matters, and the need for consilience
Markus Heilig, James MacKillop, Diana Martinez, Jürgen Rehm, Lorenzo Leggio & Louk J. M. J. Vanderschuren
volume 46, pages 1715–1723 (2021)C
………………………………………………………………….
…………………………………………………………………..
Addiction severity index
……………………………………………………………….


Leave a comment