Pathopysiology, diagnosis, epidemiology
Alcohol related liver disease accounts for significant morbidity and mortality worldwide. The 3 month mortality rate for acute alcohol hepatitis is estimated at 20-40%. Alcohol related cirrhosis accounts for approximately 25% of all cirrhosis deaths world-wide.
The spectrum of alcohol related liver disease, pathophysiology, epidemiology, prognostic indicators, and diagnostic modalities utilized are reviewed in this post.
Pharmacology of ethanol and CNS effects were discussed in an earlier post.
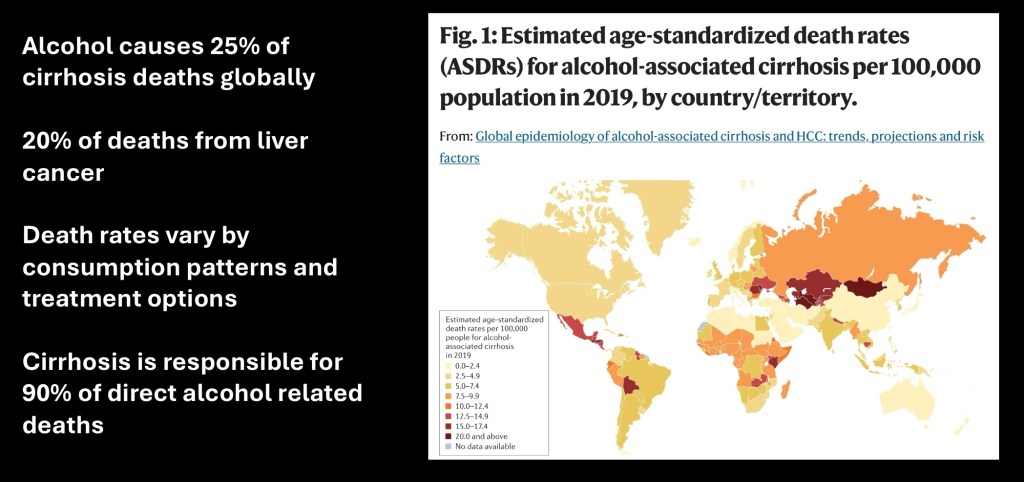
Alcohol use patterns and mortality secondary to cirrhosis vary in geographic distribution. Availability of medical treatment and diagnosis influences disease and survival rates. Approximately 20% of cases of hepatocellular carcinoma are secondary to alcohol related liver disease (ALD). Cirrhosis is the leading direct cause of alcohol related deaths.
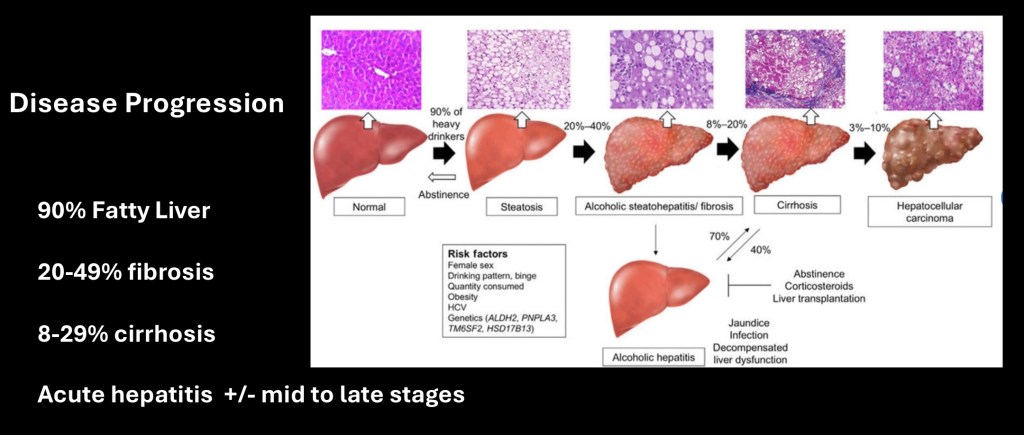
ALD is a progressive disease increasing in severity with chronic alcohol exposure. About 90% of heavy alcohol drinkers, defined as 40-60 grams per day, will develop hepatic Steatosis (fatty liver). Between 20-40% of these will develop fibrotic scarring of the liver. Between 8-20% will progress to cirrhosis which may be compensated or decompensated and 3-10% will develop hepatocellular carcinoma.
Acute alcohol hepatitis may occur at any stage and 40-50% of patients with this disease will die within 3 months even with treatment.
Abstinence from alcohol greatly improves survival and until later stages clinical reversal can occur. Hepatitis may or may not respond to treatment with corticosteroids and treatment is largely supportive care.
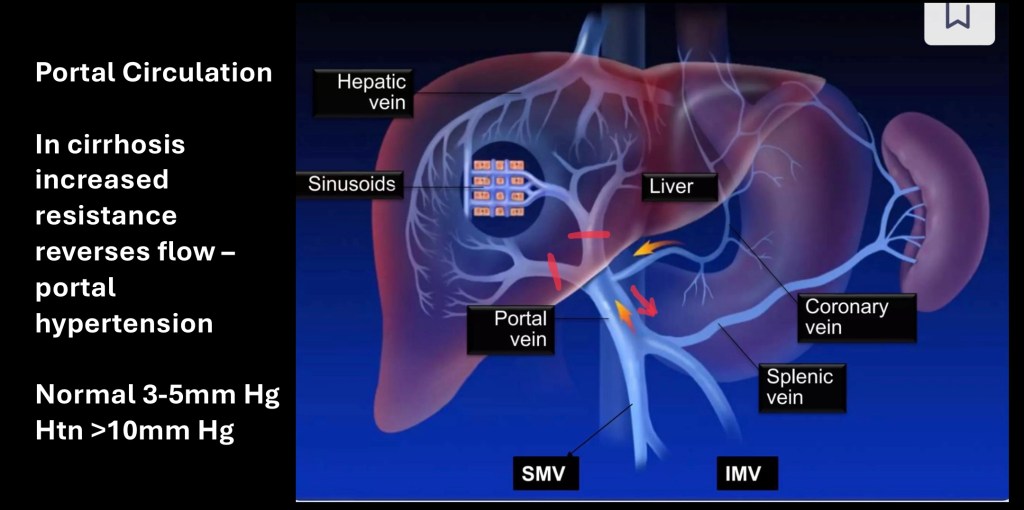
In order to appreciate liver disease, anatomy, circulation, and functional composition of the liver is essential. The portal vascular system supplies 75% of blood supply to the liver and is not directly connected to the pumping action of the heart.
The portal vessels drain from the digestive tract and spleen where, along with lymphatics, nutritional products, lipids, proteins and carbohydrates travel through the main portal vein to the liver for further processing. Alcohol is readily absorbed into the portal system and then into the liver.
The portal system is low pressure normally 3-5mm Hg. Portal hypertension is defined as a pressure greater or equal to 10mm Hg
Compare this to normal systemic arterial pressure in the 120/70 mm Hg range.
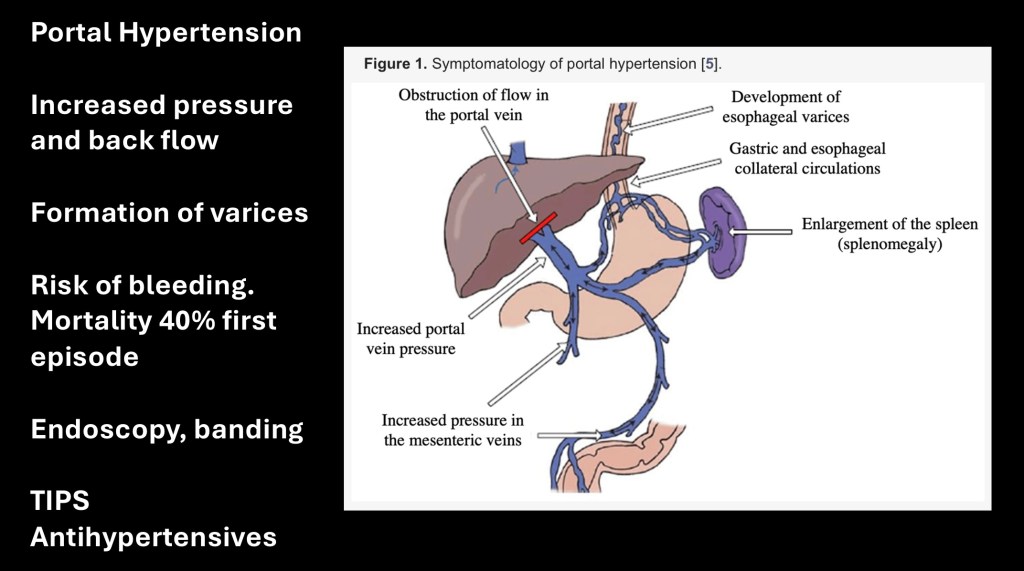
Portal hypertension is a serious complication of liver fibrosis and cirrhosis. As more fibrotic scar tissue is formed along with narrowed portal branches the resistance to blood flowing into the liver increases. A normally low pressure system without a pump results in back flow away from the liver. The weakened vascular walls become dilated and tortuous (varices) Collateral circulation may form.
The varices are prone to rupture with internal bleeding. About 40% of first time bleeds result in death. With endoscopy, banding of varices in the lower esophagus may prevent rupture. Enlargement of the spleen (splenomegaly) may occur which can result in splenic infarctions. Antihypertensive agents can improve survival time.
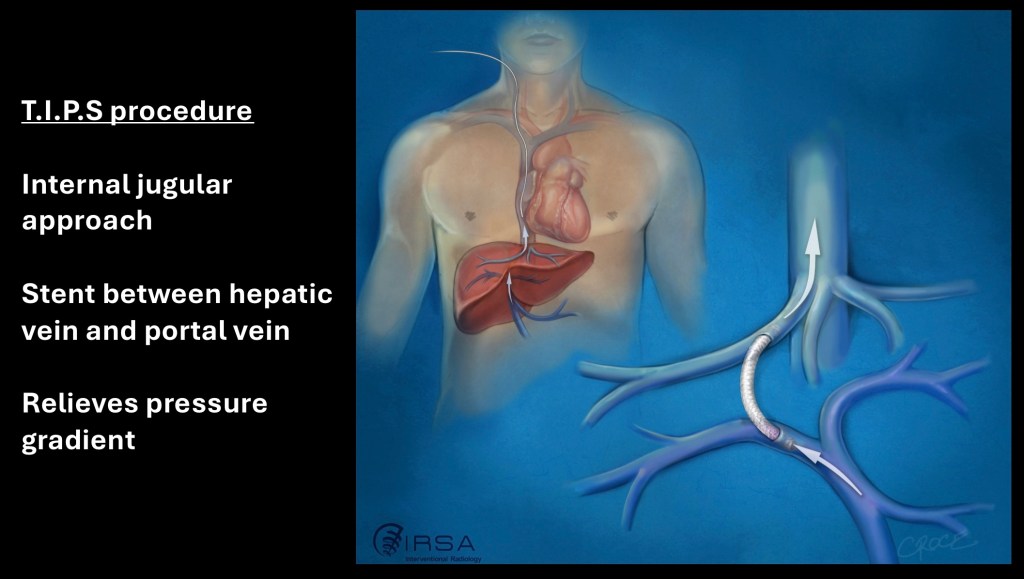
T,I.P.S. Procedure may be used in some patients to lower portal pressure and prevent further disease progression. Transjugular Intrahepatic Portal Systemic Shunt involves introduction of a catheter down from the internal jugular vein into an intrahepatic systemic vein in the liver. A channel is then formed from the hepatic vein into a neighboring portal vein and an artificial metallic shunt tube is placed.
With the TIPS in place portal pressure is relieved. Complications may include stenosis (narrowing) of the shunt and increased hepatic encephalopathy.
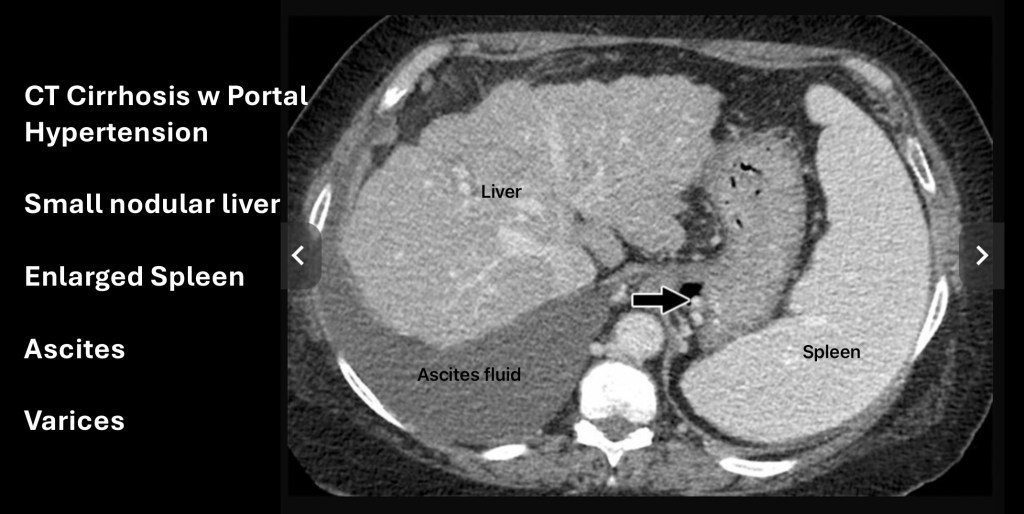
This is a CT scan of the upper abdomen following IV contrast in an individual with cirrhosis. To the left on the image (anatomic right) the liver is smaller than normal. The liver has a nodular contour. The margins are normally smooth. This is due to scar tissue and volume loss.
Just adjacent to the liver toward the bottom of the image is darker grey material. This is ascites, a buildup of free fluid in the abdomen which may need to be drained periodically if persistent.
On the opposite side is the spleen which is enlarged (splenomegaly). It should be smaller than the liver.
The arrow points to small rounded bright structures. These are varices at the lower esophagus where it joins the stomach.
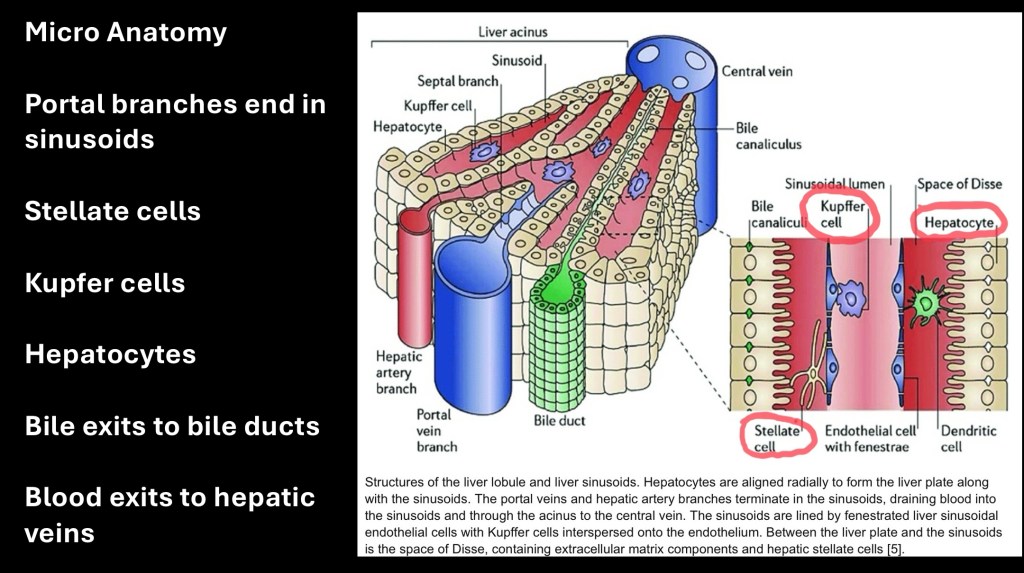
Anatomy and functional structure of the liver is essential to understanding pathology of liver disease. Blood flow enters the liver through the portal veins (75%) and hepatic arteries (25%). After filtering through hepatocytes it collects to the hepatic veins and back into the systemic circulation. Bile formed by hepatocytes collects into bile ducts which drain into the duodenum to aid in digestion.
Sinusoids are the smallest terminal branches. They are lined by epithelial cells, kupffer cells, and stellate cells. Each of these are damaged by alcohol and contribute to ALD. Sinusoids are surrounded by sheets of hepatocytes which are the principle functional cells in the liver. Blood flowing out drains through the hepatic veins into the systemic circulation.
The liver may be thought of as a chemical factory taking raw materials and assembling them into finished products necessary for life. It also functions to handle toxins through various pathways. Ethanol is one of those and damage occurs when intake exceeds the ability to metabolize alcohol and by products.
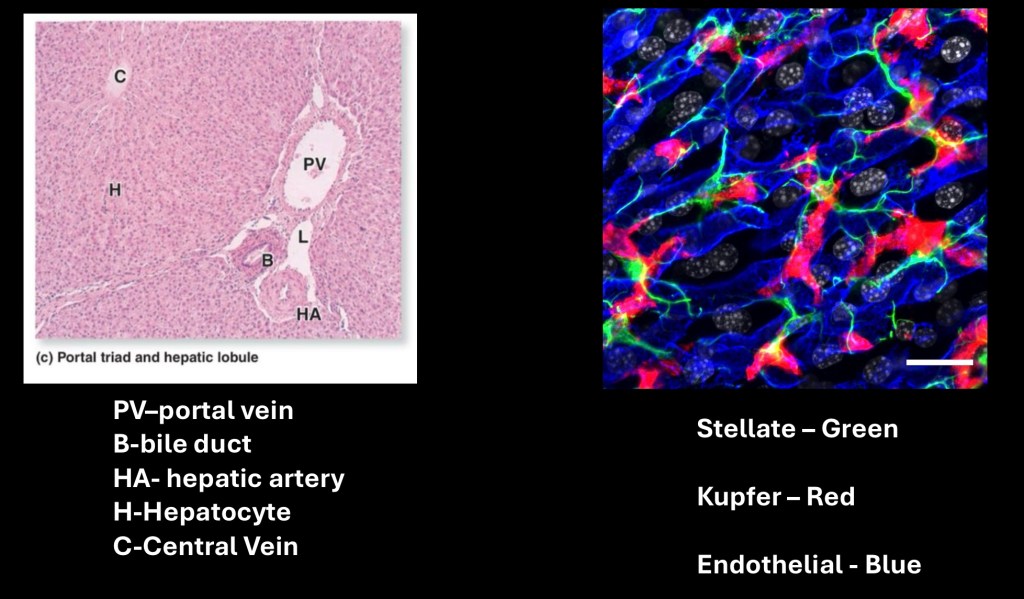
On the left is a micrograph of a section of liver with labeled components. The majority consists of sheets of hepatocytes forming a lobule. These are separated by the vascular triad consisting of a Portal Vein, Hepatic Artery, and Bile Duct. In the center of each lobule is a hepatic vein separate from the other structures.
On the right are fluorescent labeled Stellate cells (green), kupffer cells (red) and Endothelial cells (blue). These line the sinusoids and are further discussed below.
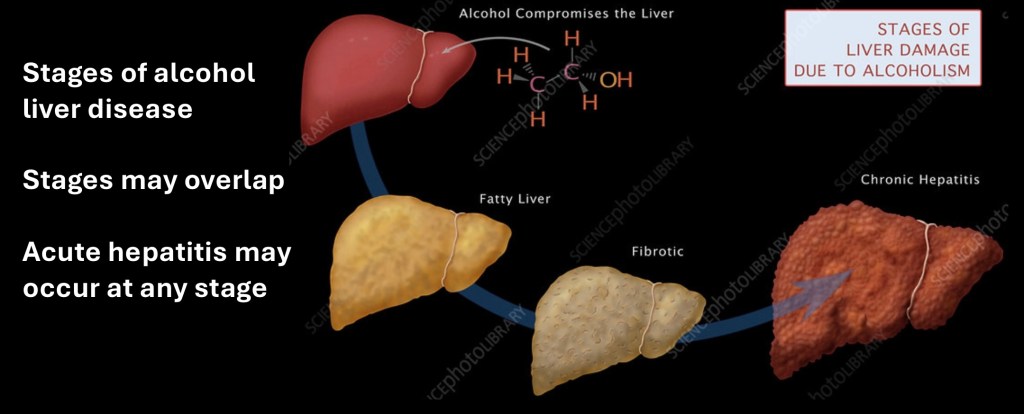
Chronic Alcohol Liver disease follows a predictable pattern from normal to fatty liver and then to increasing degrees of fibrosis, inflammation and cirrhosis. Acute hepatitis is an inflammatory condition which may occur in different stages of ALD.
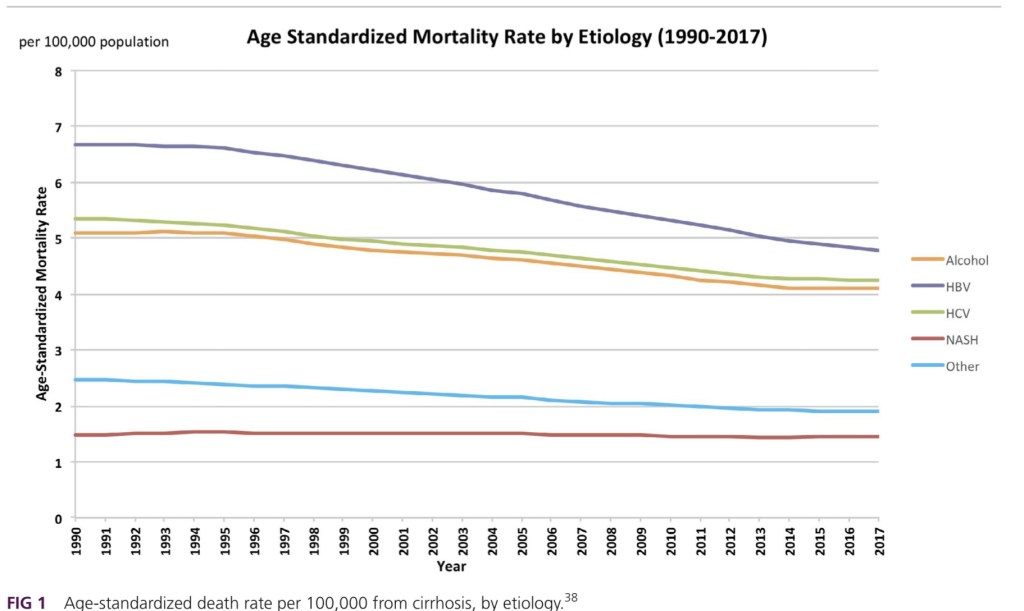
Worldwide chronic liver disease is a leading cause of morbidity and mortality. This graph represents age adjusted mortality rates for the major causes of hepatitis. Hepatitis B viral infection has been the most common cause followed by Hepatitis C. These have been declining due to improved prevention and treatment measures. Most common causes are viral hepatitis followed by alcohol related liver disease and then Non Alcoholic Steatohepatitis.
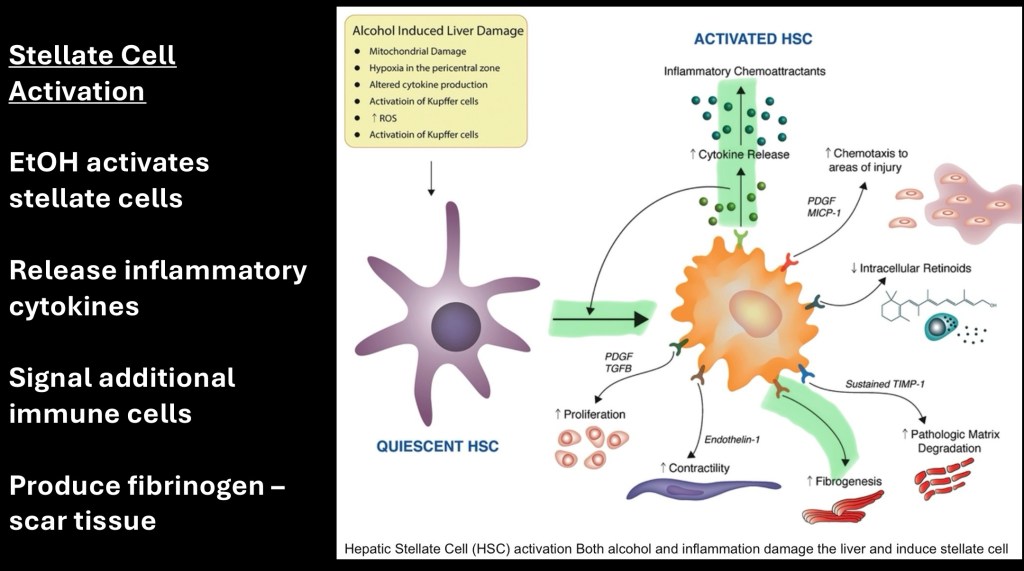
Stellate cells (SC) line hepatic sinusoids. Normally these cells are quiescent and function in retinol storage and a few other activities. Chronic alcohol exposure activates these cells. In the activated state SCs proliferate. They produce fibrin which coalesces into scar tissue. SCs produce cytokines recruiting inflammatory cells and reactions.
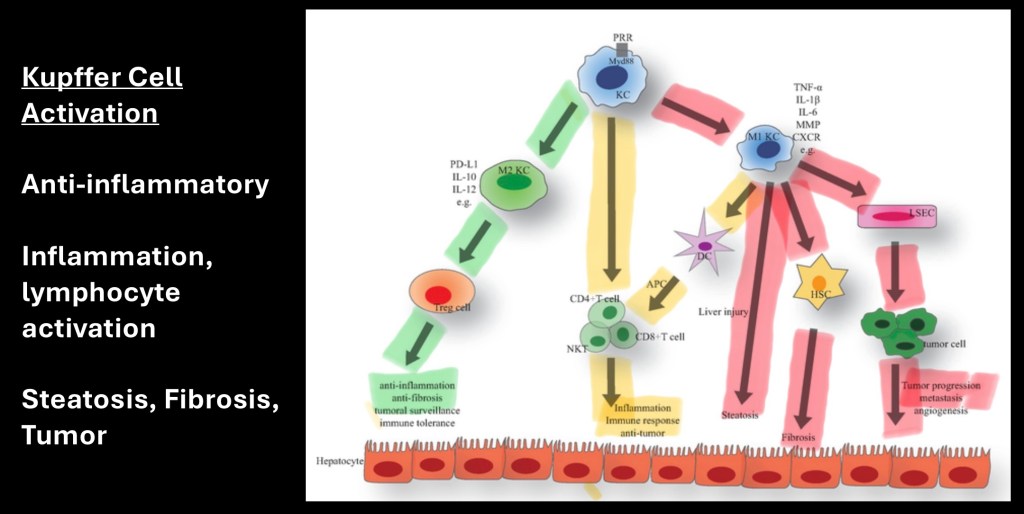
Kupffer cells (KC) are liver macrophages. They function in protection and defense from infection and other threats. The above diagram shows three pathways which may occur when KCs are activated.
Shown in green KCs act in an anti-inflammatory capacity. They decrease fibrin accumulation and function in tumor surveillance.
In yellow shown is activation resulting in recruitment of T-lymphocytes and natural killer (NK) lymphocytes. This results in an inflammatory reaction and may result in tumor suppression and immune response.
Shown in red is release of Tumor Necrosis Factor (TNFα), Interleukins, and other factors produced by Kupffer cells. This leads to fibrogenesis, stellate cell activation, cellular destruction, and tumor growth.
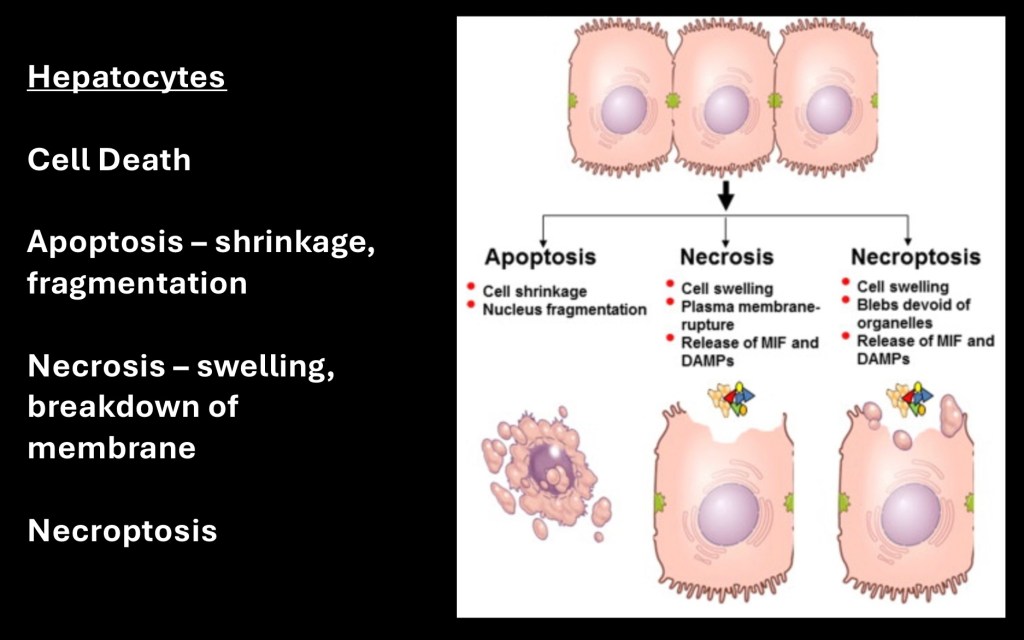
Liver hepatocyte damage and cell death may occur in several ways. Apoptosis refers to a process in which the cell shrinks in size. The cell nucleus and cytoplasm become fragmented breaking into smaller pieces.
Necrosis refers to a process whereby the cell swells. The membrane becomes disrupted releasing cell contents into the extra cellular space. In necropoptosis cellular swelling and fragmentation both occur. In each of these processes the result is cellular destruction and loss of functional liver tissue.
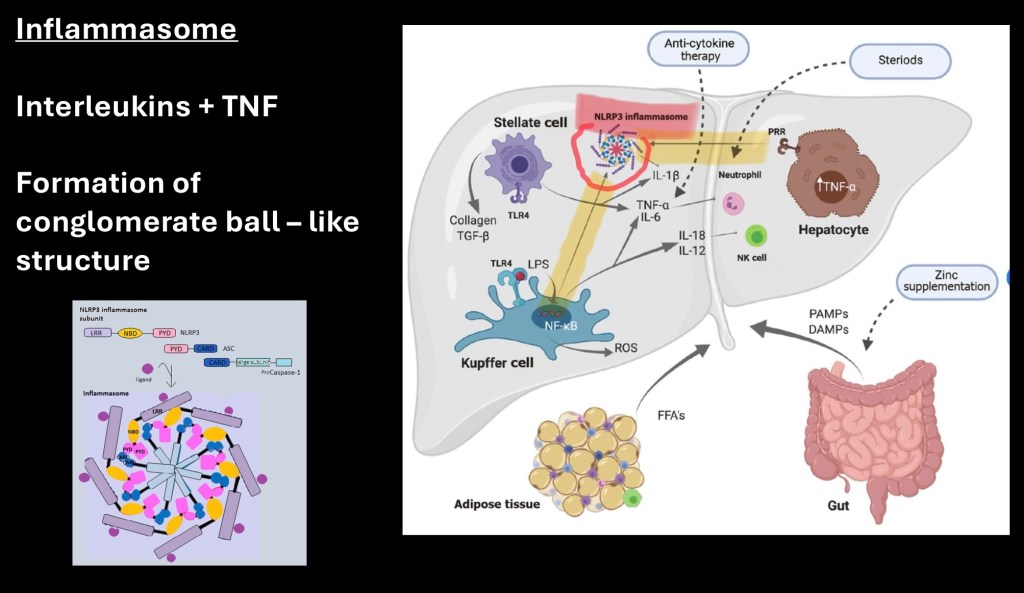
Inflammasomes are conglomerate proteins and inflammatory factors forming a ball-like structure seen in advanced ALD. These are a result of combined cytokines and interleukins along with cellular contents furthering destructive cell processes.
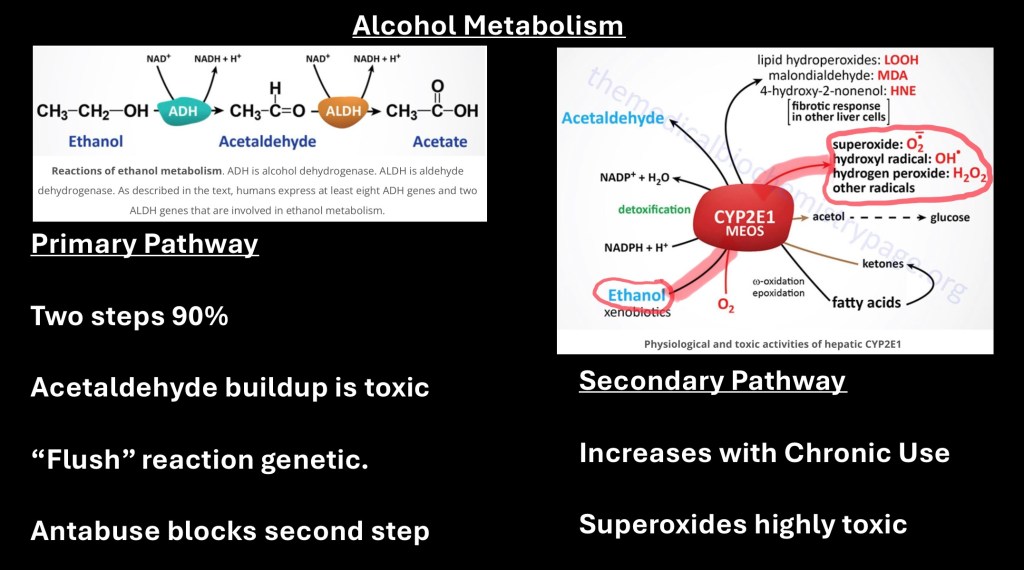
Alcohol metabolism in the liver occurs by two principal pathways. 90% of alcohol is metabolized in the liver with a fraction broken down as blood containing alcohol passes through with each cycle.
The principal pathway is a two step enzymatic pathway. Ethanol is first converted into acetaldehyde which is then converted in a second step into acetate. Acetate can be converted into energy in the tissues by the citric acid cycle leaving carbon dioxide and water.
Acetylaldehyde is toxic and can build up resulting in cellular toxicity. There are genetic variants of the two enzymes involved ADH and ALDH some of which are less efficient leading to individual variation in levels of circulating alcohol and acetylaldehyde.
The second pathway seen above is by CYP2E1. This is in the cytochrome P450 family of enzymes. Under normal conditions this pathway contributes 10% or less of total alcohol metabolism. However in chronic use as adaptive changes occur due to high circulating alcohol levels this pathway upregulates and becomes the primary metabolic pathway.
This reaction is highly toxic producing reactive unstable oxidants such as hydrogen peroxide and nitric oxide. This results in damage to DNA and cellular structures leading to cell death.
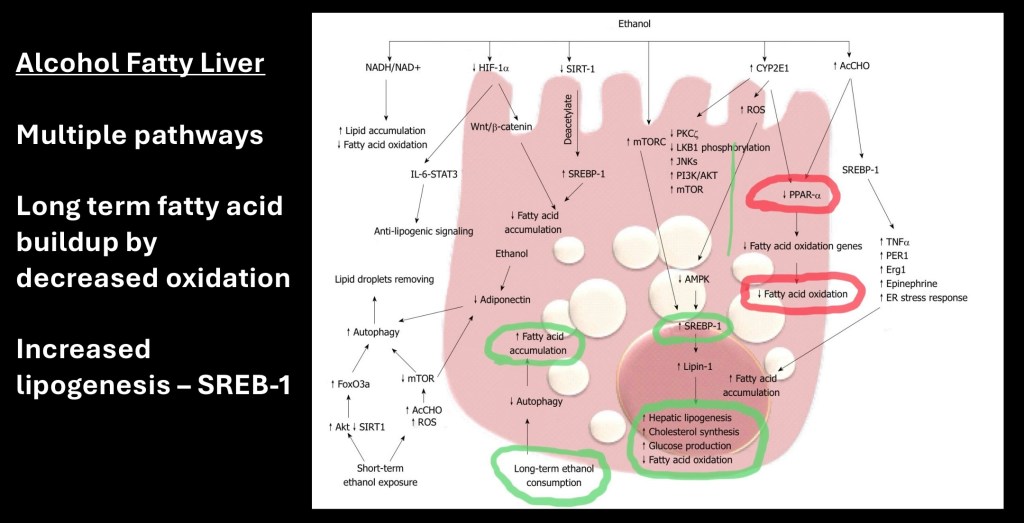
Fatty accumulation in the liver is the result of multiple metabolic changes. One is by increase in lipogenesis, increased fatty acid and glucose production. In addition there is decrease in normal oxidation of fatty acids. The result is buildup of intracellular fats.
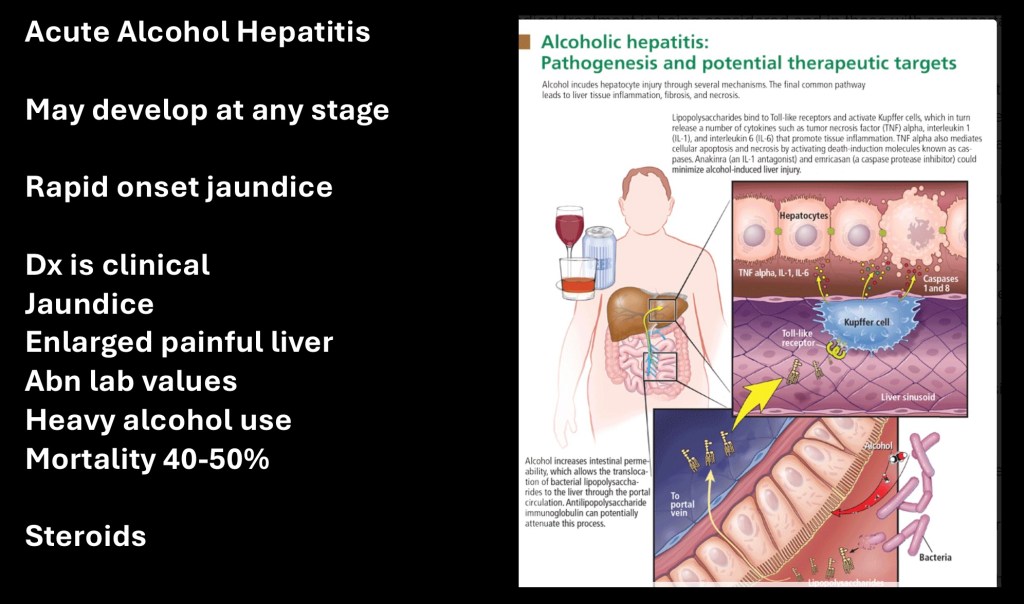
Acute alcohol hepatitis may occur at any stage. It has poor prognosis with mortality rate from 50-60%. Diagnosis is clinical with rapid onset of jaundice and liver tenderness. Encephalopathy, hepatorenal syndrome, encephalopathy, ascites, edema and abnormal lab values are clinical signs and symptoms.
The most effective treatment is cessation of alcohol. Steroids may be helpful. Liver failure may progress to multi system organ failure.
The primary mechanism is kupffer cell activation. Generation of cytokines including tumor necrosis factor α and interleukin 1 result in hepatocyte inflammation, apoptosis, and necrosis.
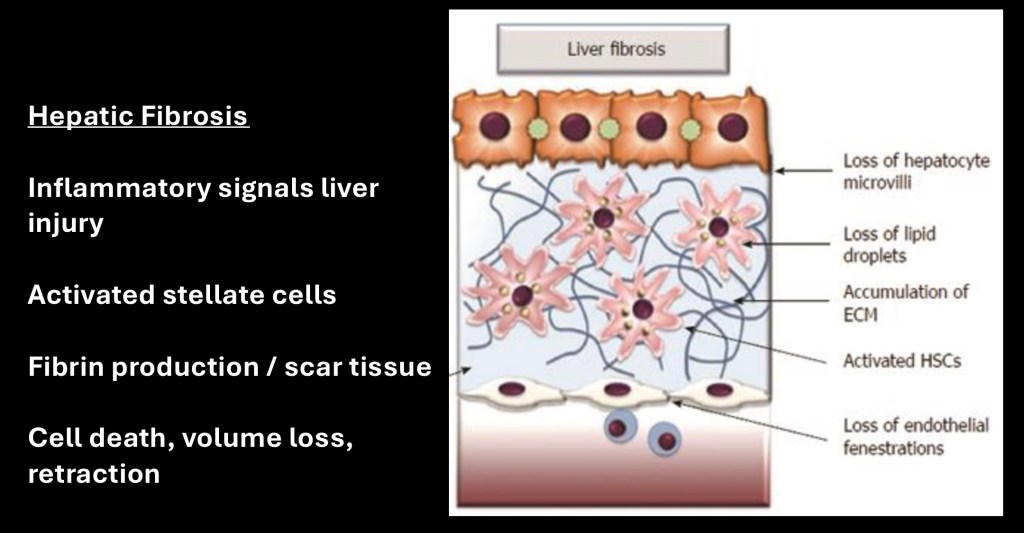
Over time liver fibrosis dominates the disease process. Activated stellate cells produce fibrin which collects into scar tissue. Fatty changes decrease with progressive fibrosis. Damage to lining endothelial cells and hepatocytes further contributes to decreased function, metabolic abnormalities, and loss of liver tissue. With continued alcohol use higher blood alcohol levels result in multi organ failures.
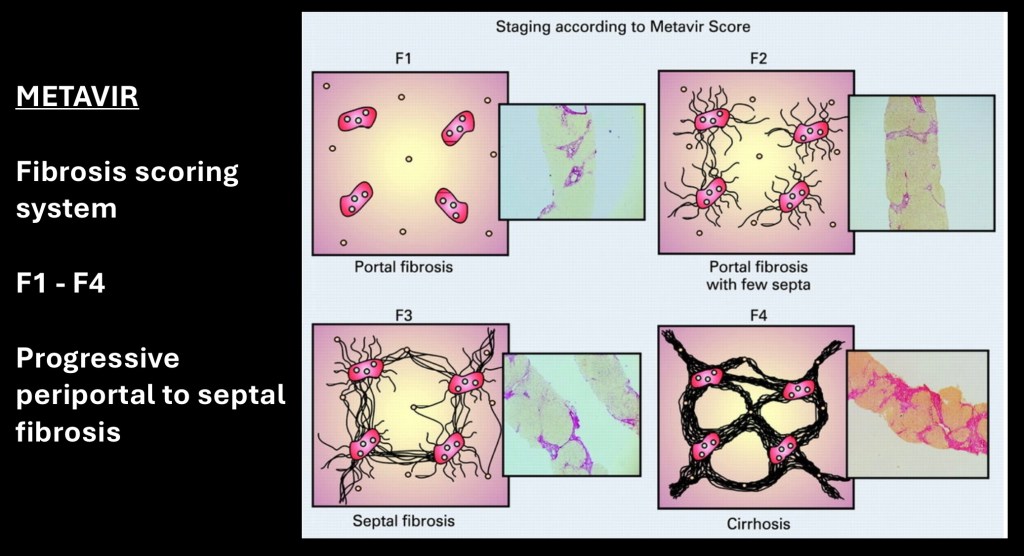
METAVIR is a grading system for fibrosis and cirrhosis based on histologic features on liver biopsy. F0 is normal and changes are graded to F4 cirrhosis. Fibrotic changes are first seen in the peri portal region. Later fibrosis occurs in the septa around cells with markedly thickened fibrosis and cell destruction in later disease.
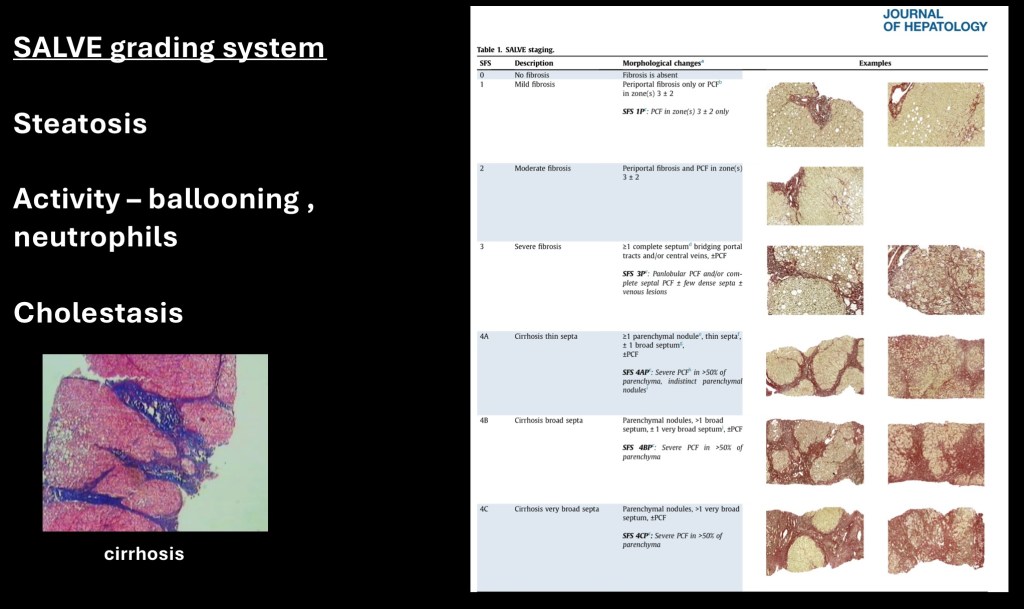
A number of prognostic grading systems have been developed. The SALVE histopathologic grading system was developed in Europe. In addition to fibrotic changes it incorporates fatty liver changes and inflammatory cells to come up with a more comprehensive risk and prognostic indicator.
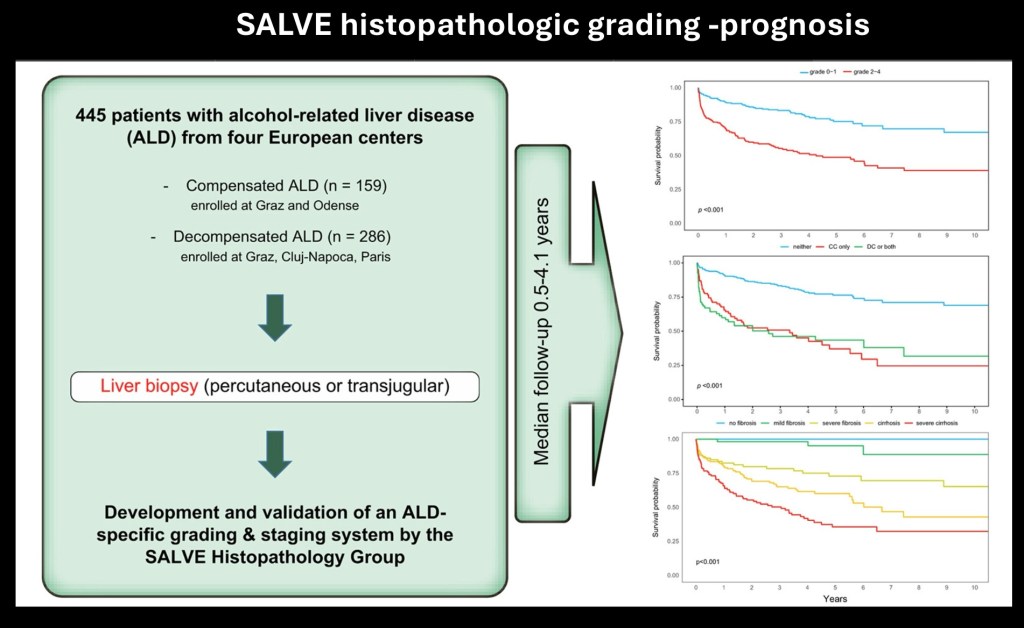
Multi center long term follow up was performed using the SALVE criteria. Survival curves were generated indicating ten year prognosis. From top to bottom survival curves for grades 0-1/2-4, compensated/decompensated/neither/both, and no fibrosis to severe cirrhosis.
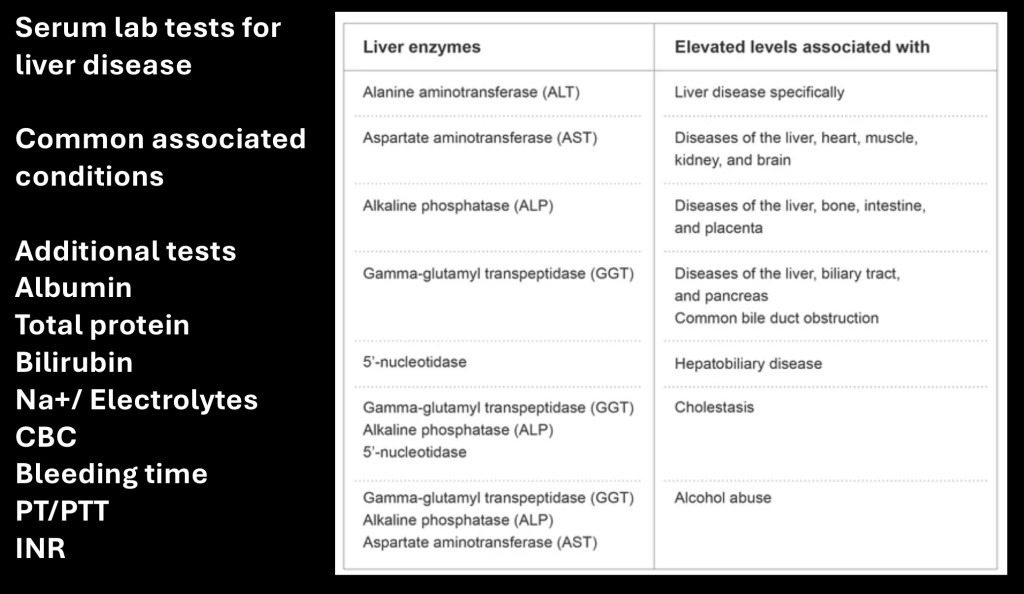
Serum blood tests are a routine essential component in diagnosis of ALD. Treatment options including indications for transplant are guided by lab values. These are often combined in a standard liver panel. Common serum levels are listed above along with relevant clinical significance.
ALT- Alanine aminotransferase. One of the group of enzymes involved in protein synthesis
AST – Aspartate aminotransferase
ALP – Alkaline phospatase. Enzyme present in liver, bone and other tissues.
GGT – Gamma glutamyl transpeptidase. Enzyme found throughout the body. Highest within the liver. Most sensitive for acute alcohol consumption.
Additional tests include CBC (complete blood count), coagulation tests (PT, PTT, INR international normalization ratio) electrolytes (Na+, K+, Cl-,Ca++) Albumin and total protein, and bilirubin.
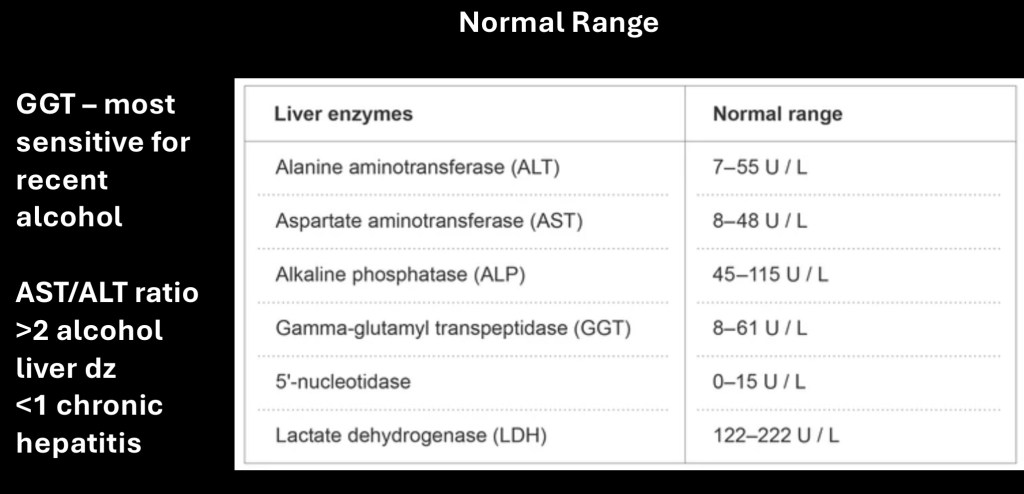
Typical normal ranges are listed above although individual labs may use different ranges.
The AST/ALT ratio is a useful parameter when levels are abnormally elevated. A ratio >2 indicates alcohol related liver disease. A ratio <1 indicates chronic hepatitis.
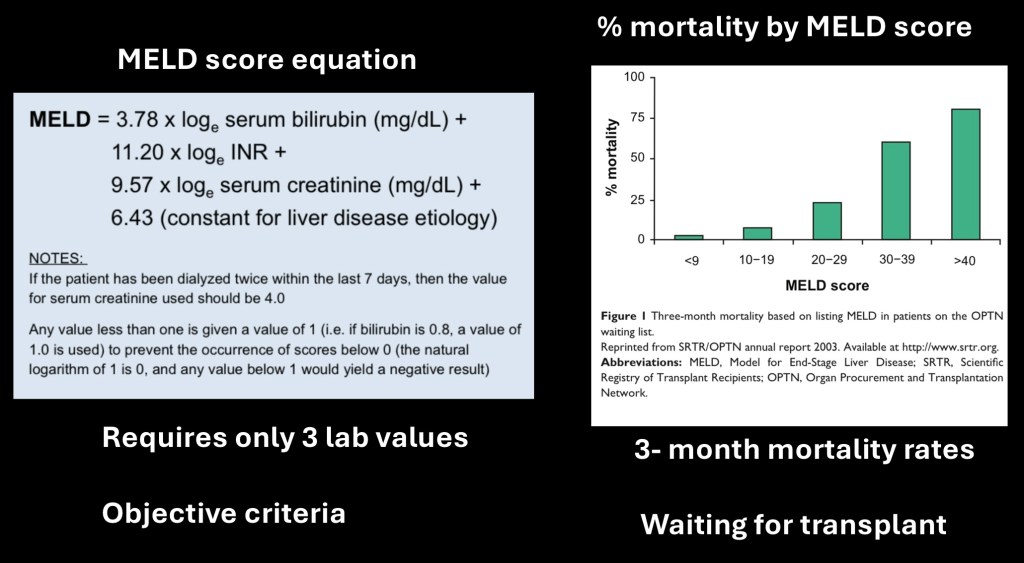
The MELD score was originally developed at the Mayo Clinic to determine which patients were likely to benefit from a TIPS procedure. MELD stands for Mayo End Stage Liver disease. The original formula has the advantage of only requiring three common lab values, using only objective criteria, and has a high prognostic value. The equation is listed above.
The chart on the right shows expected 3 month mortality by MELD score.
Soon after the scoring system was evaluated it was adapted for use in assessing which patients were most likely to benefit from liver transplant. Due to its objective parameters and high prognostic specificity it has become widely used. Some variations from the original formula are in use.
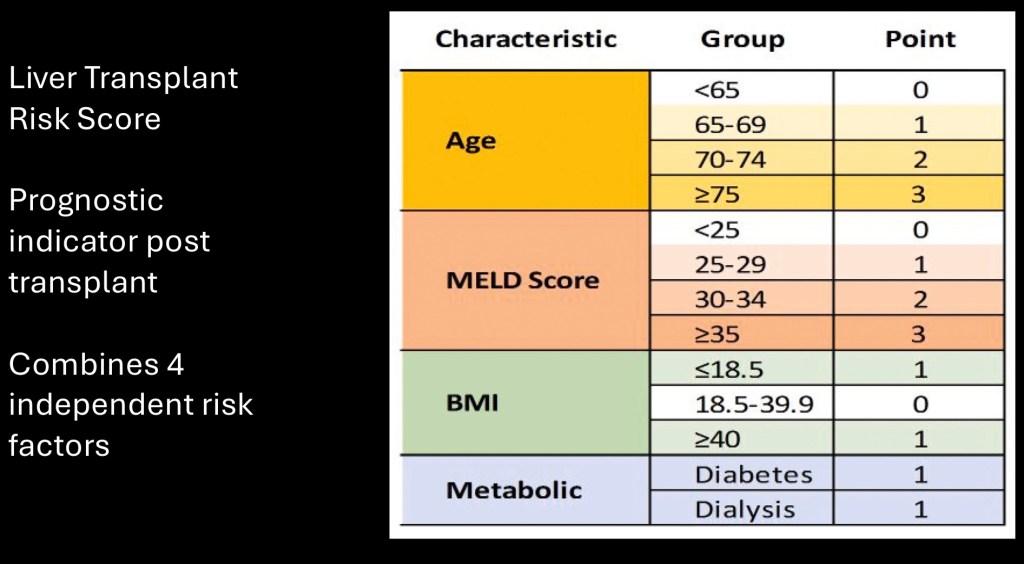
The LTRS scoring system above has been developed to assess post transplant prognosis. In addition to MELD score it includes age, body mass index, and diabetes status.
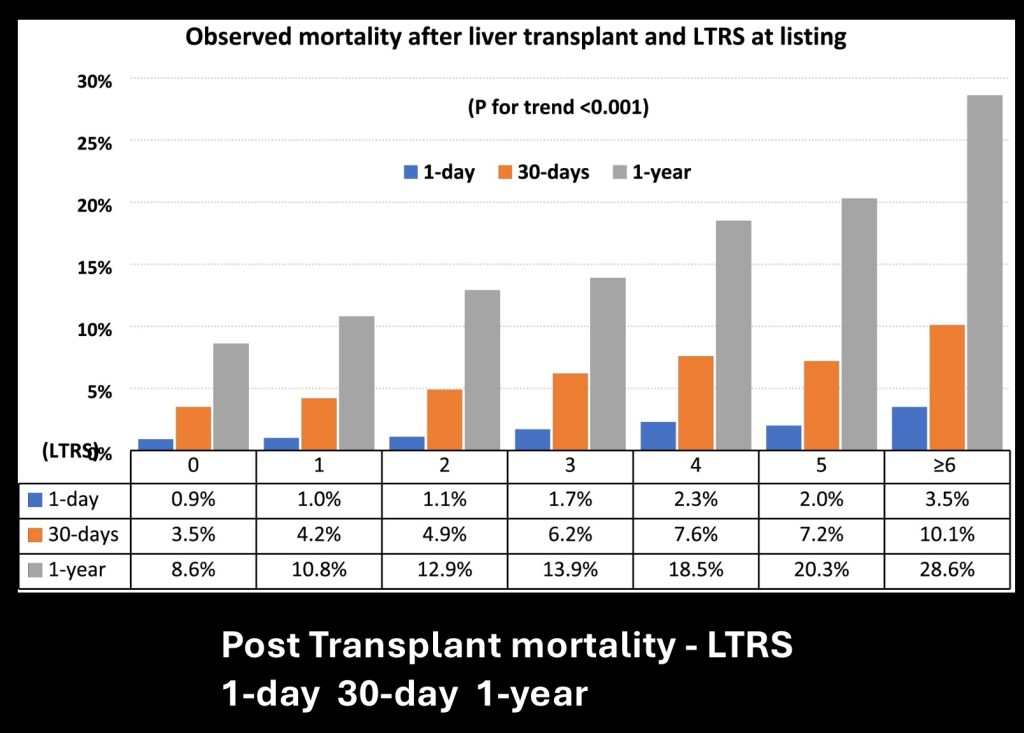
This chart shows expected mortality post transplant using LTRS scoring. Data are given for 1- day, 30-day, and 1-year. Scoring is from zero to six or greater.
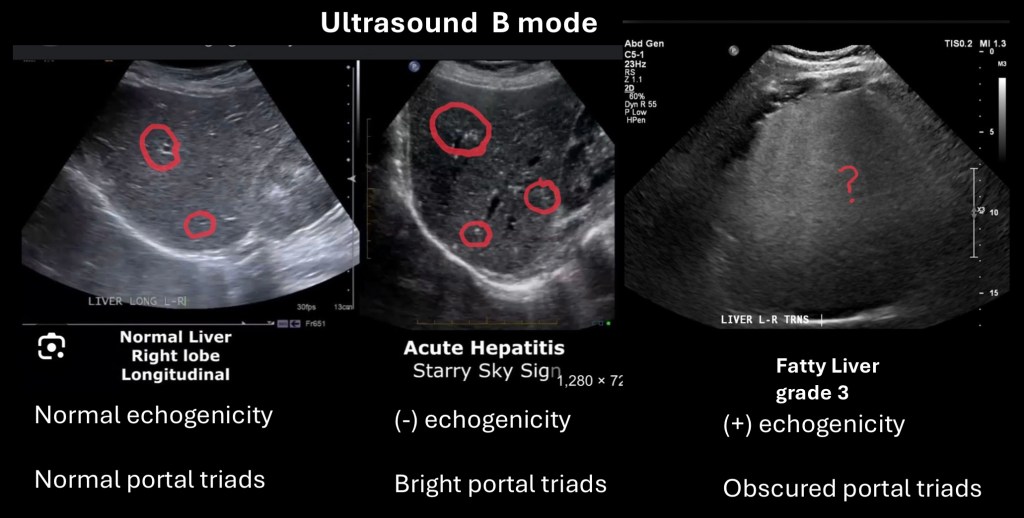
Imaging is a key component for evaluation of liver disease. Standard B-mode ultrasound is qualitative rather than quantitative. It is operator dependent and interpretation is largely subjective. It has the advantage of lower cost and no ionizing radiation compared to MRI or CT.
Echogenicity is a descriptive term for ultrasound. High echogenicity structures will appear brighter. Low echogenicity structures will appear darker.
Evaluation for steatosis has a sensitivity of 68,4% and specificity of 75%. Using graded ultrasound criteria improves diagnostic accuracy.
The “starry sky” appearance is when the liver becomes hypoechoic and bright portal triads appear more prominent. It is thought to be associated with acute hepatitis. However this sign has been shown to have low specificity and sensitivity. Ultrasound has high value in identifying presence of gallstones, dilated bile ducts, spleen size, most cysts or masses, and presence of ascites.
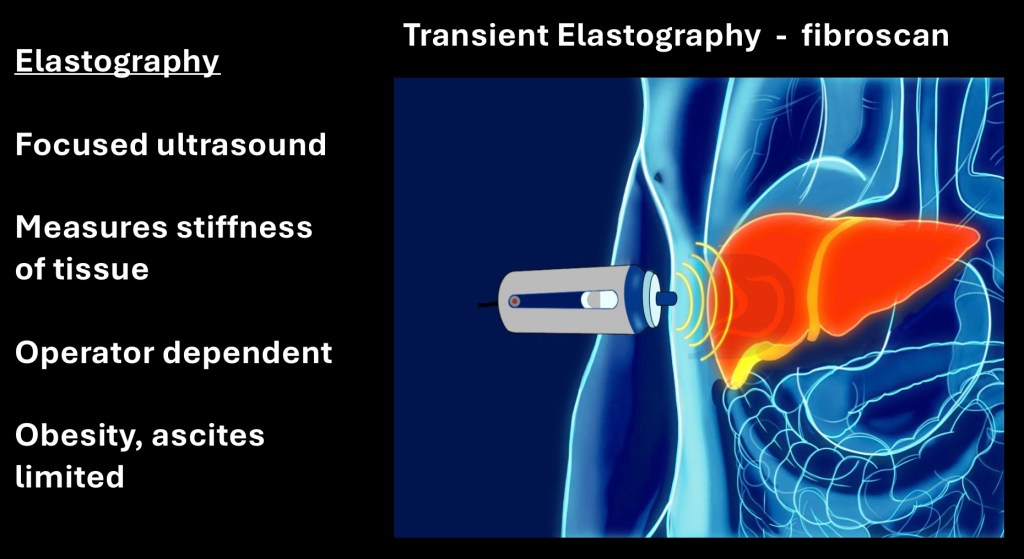
Transient elastography is a focused ultrasound technique which has been developed to give a quantitative measurement of liver stiffness related to fibrosis. Fibroscan is a leading commercial product developed by Echosence a company located in Paris, France.
The technology takes advantage of a pressure wave generated by sound as it passes through tissue resulting in compression. The relative stiffness of the tissue will be reflected in minute deformation generated by the ultrasound wave. Stiffer tissue is less “squishy”.
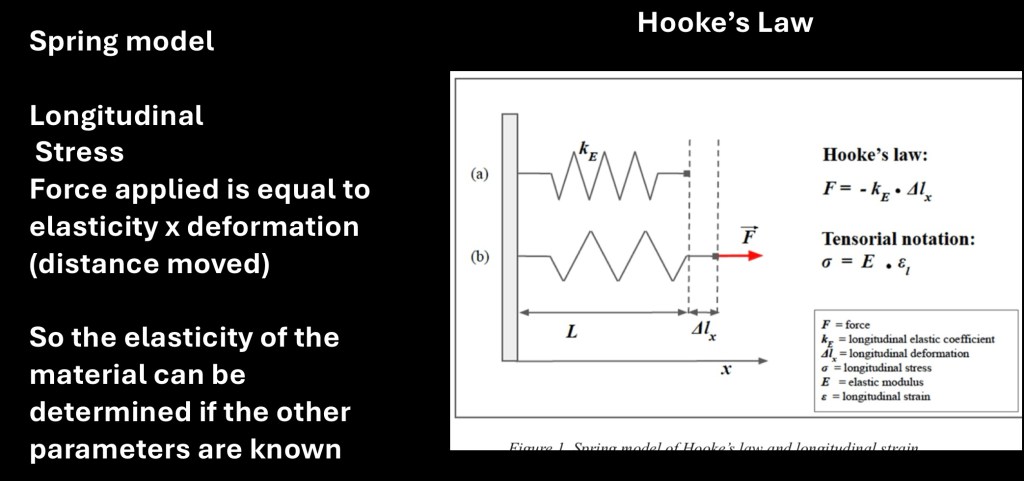
A simplified model of the physics involved. Hooke’s law states that force applied is proportional to the elastic coefficient and longitudinal deformation. From this information a measure of elasticity can be obtained expressed in kPa/m2, (kilo Pascals per unit area).
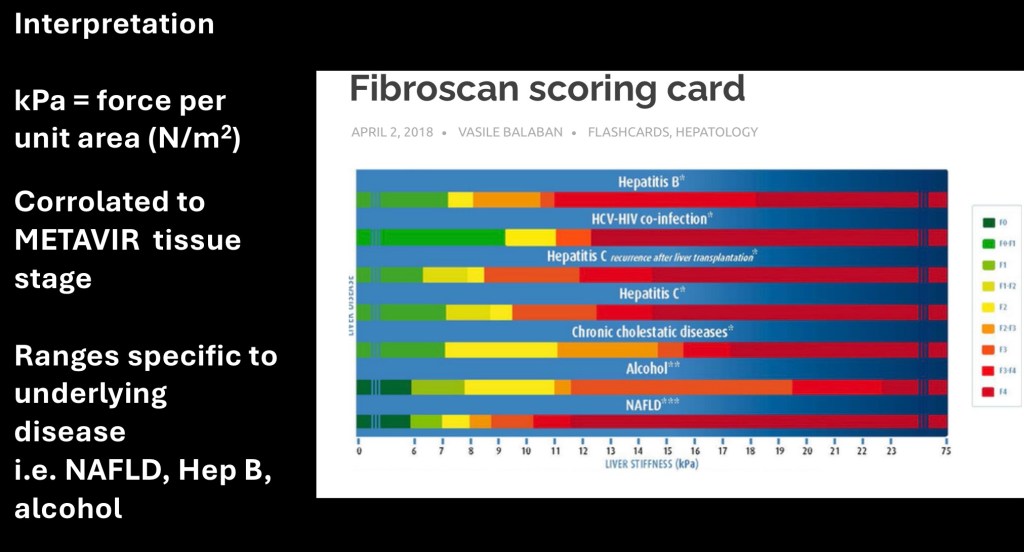
The derived measurement has been compared with biopsy findings to correlate with fibrotic METAVIR stages for differing liver pathologies such as alcohol, hepatitis B, and other causes. The result is a non invasive method to determine fibrotic change due to liver disease.
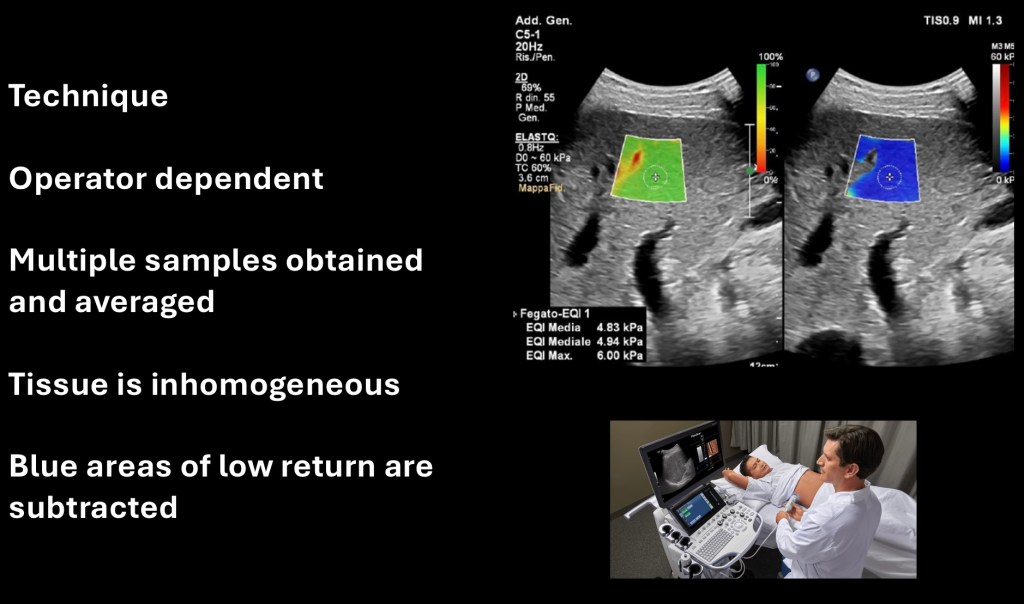
Multiple sampled areas are obtained and averaged to arrive at a representative measurement. Liver tissue and disease pattern is not uniform. The picture at the top represents in green an area to be sampled. Red to yellow areas are non uniform such as a passing blood vessel and will not be included in the sample.
The blue area is where a measurement will be obtained. Note the red/yellow areas are blacked out. At least 6 measurements should be obtained and averaged.
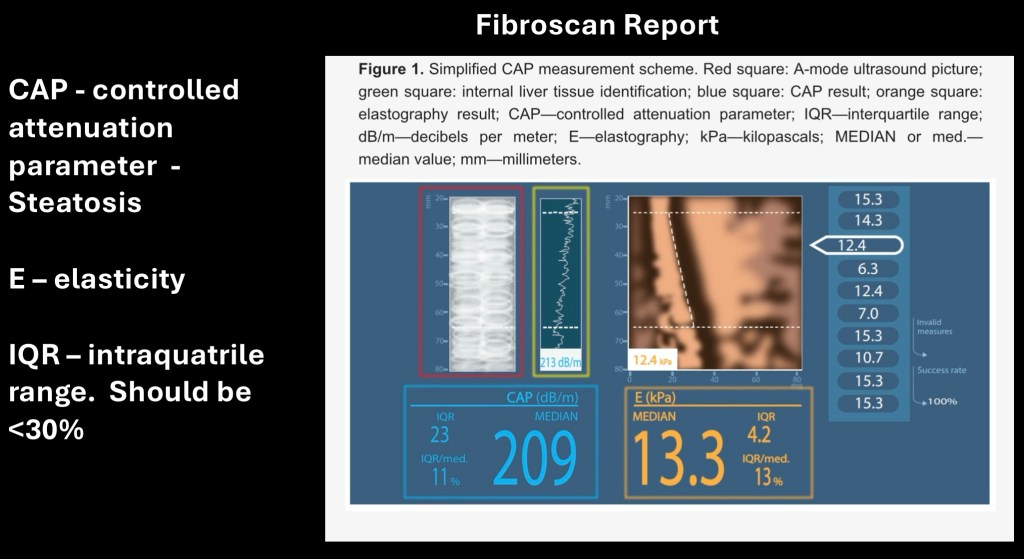
A sample Fibroscan report. The orange box is the stiffness measurement to be correlated with known values corresponding to fibrotic stage. The blue box is the controlled attenuation parameter (CAP) representing grade of fatty change present.
The IQR (interquartile range) indicates variability and should be <30%. High IQR may indicate a non diagnostic scan.
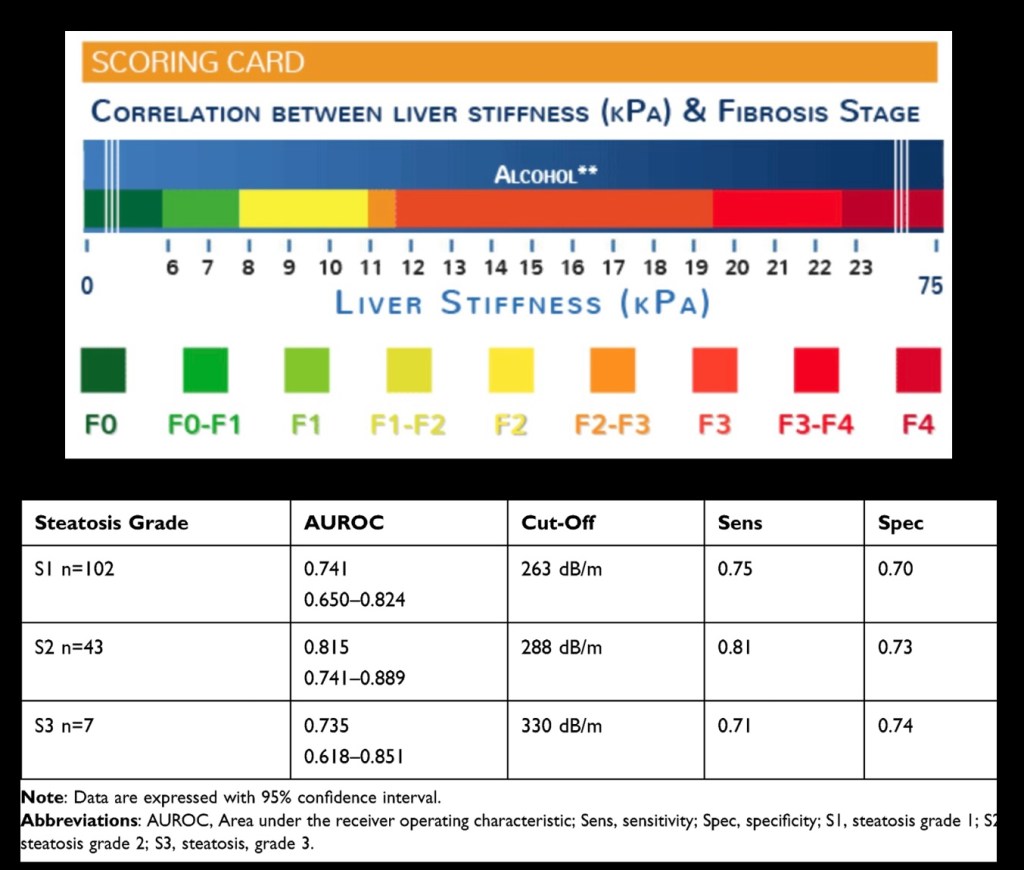
The topmost scale represents fibrosis stage and stiffness measurement for alcohol liver disease. The table at the bottom indicates sensitivity and specificity of CAP Steatosis grade obtained from Fibroscan. Results from other equipment manufacturers may differ and may not be directly comparable.
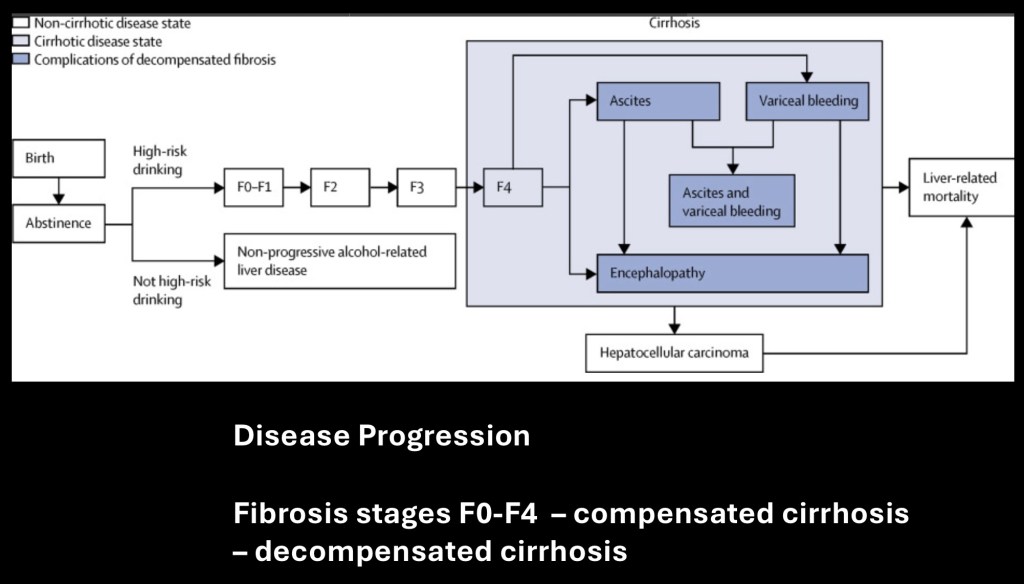
Flow chart of disease progression through fibrosis to stage 4 compensated cirrhosis followed by decompensated cirrhosis (dark blue), Decompensated cirrhosis is manifested by encephalopathy, ascites, bleeding varices and in some cases hepatocellular carcinoma.
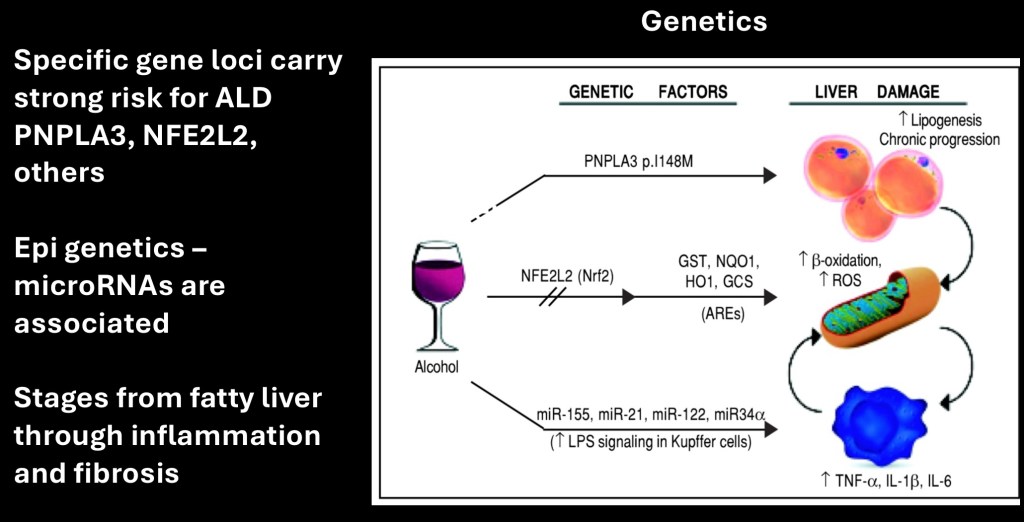
Genetic and epigenetic factors have been demonstrated to have a role in development of ALD. Variant versions of the PNPLA3 gene and others are linked to cirrhosis. Micro RNA epigenetic mechanisms play a role in disease progression. These are thought to participate in Kupffer cell activation and lipopolysaccharide signaling.
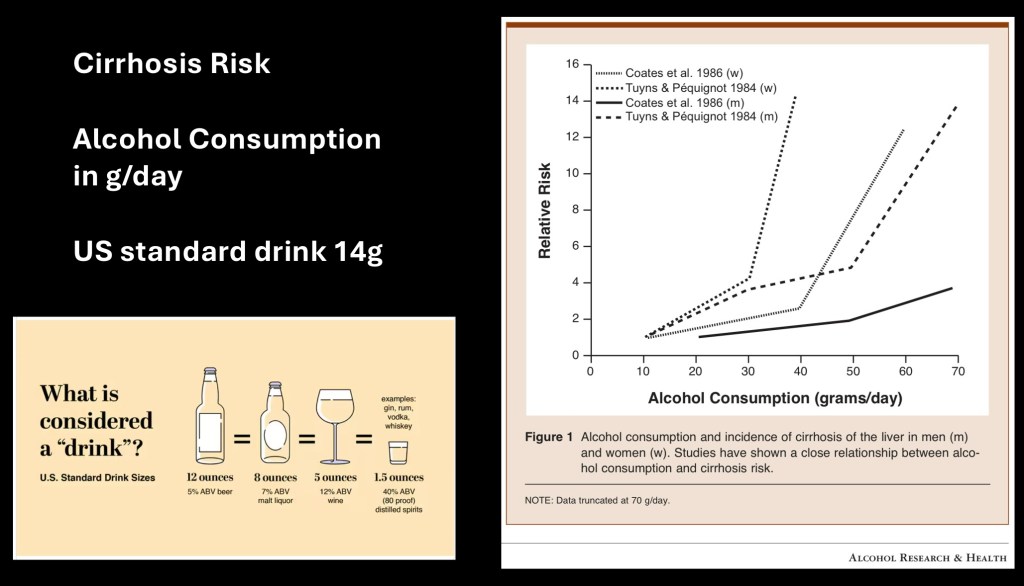
The graph on the right shows relative risk of ALD at different daily consumption levels. Risk sharply increases at 40g/day. A standard US drink is considered to contain 14 grams of alcohol. Equivalents for different beverages are shown on the left. Time to disease onset is variable. Ten years of heavy drinking would be an approximate estimate.
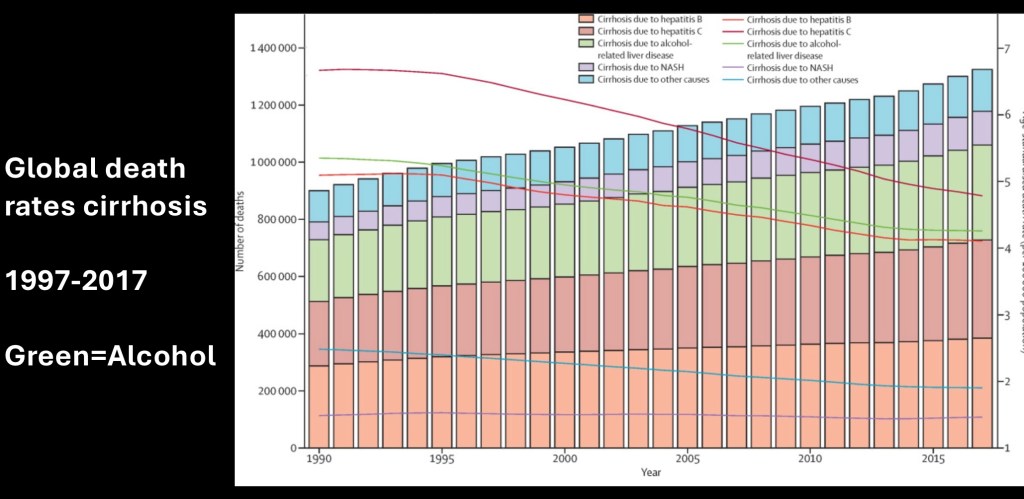
Global cirrhosis death rates by cause 1990-2017. Total number of deaths is largest for Hepatitis B and C. Alcohol is the third leading cause. Adjusted death rates are trending down. Alcohol is in green. Bars represent total deaths. Lines represent deaths/100,000 population.
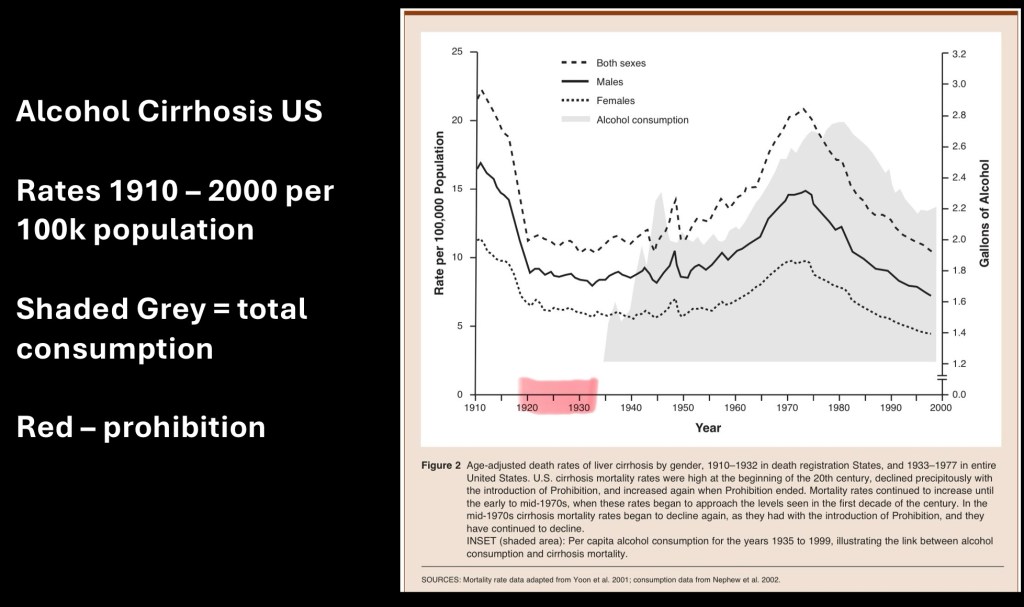
This graph represent historical death rates due to alcohol cirrhosis 1910-2000. The solid grey shaded area represents total national alcohol consumption.
Red highlights are the years of alcohol prohibition in the US. A dramatic drop is seen in cirrhosis incidence during prohibition with a gradual increase following repeal. Data are separated by male, female, and total.
Note a peak in the mid 1970s followed by decrease trend extending to 2000.
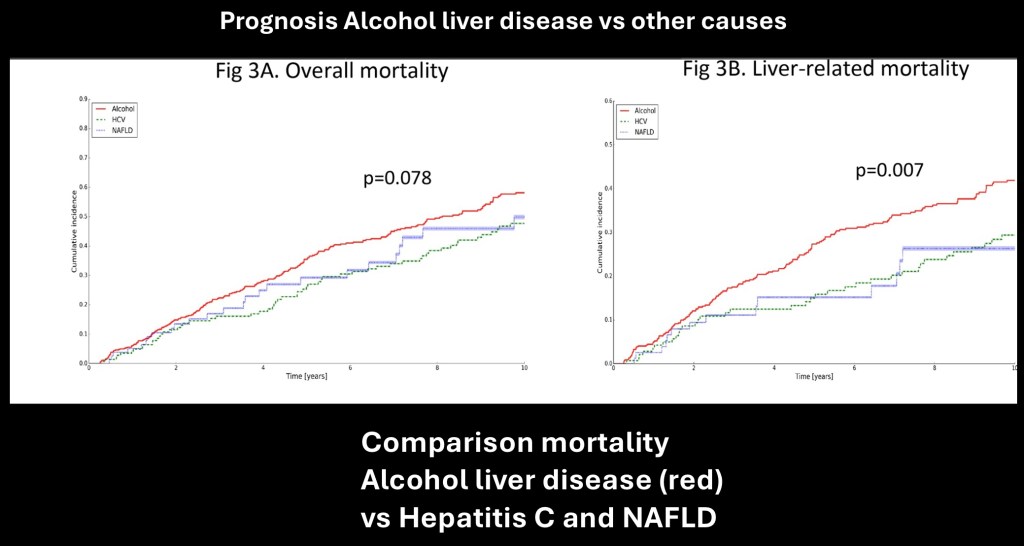
Alcohol related liver disease has a worse prognosis than cirrhosis due to hepatitis C and NAFLD. The three groups are similar in overall mortality over a 10 year period. The alcohol group (red) had a significantly higher liver related mortality rate.
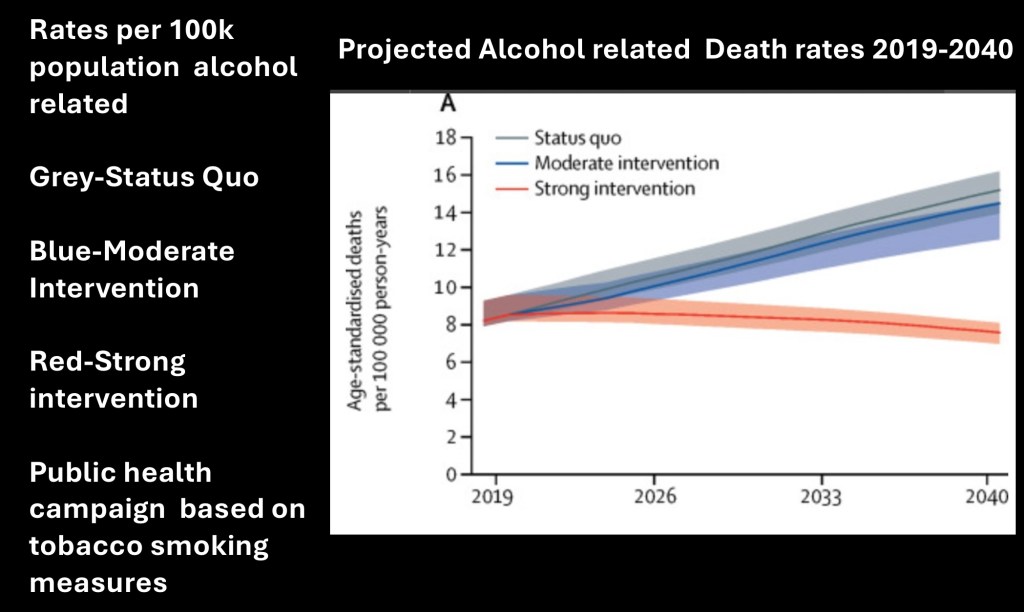
This study utilized existing data to construct a predictive model for projected ALD mortality into 2040. Three different scenarios were included, status quo, mild intervention, or strong intervention. Intervention was defined by anti tobacco public health measures applied to alcohol.
The strong intervention model (orange) projected a significant decline in mortality compared with the other groups with around 50% fewer deaths by 2040.
………………………………………………………………….
Alcohol related liver disease is a significant cause of morbidity and mortality in the US and throughout the world. Alcohol toxicity results in changes in hepatocellular structures, fibrosis, cell death and damage, and inflammatory responses. Diagnosis and grading is aided by imaging studies including ultrasound and transient elastography. Serum lab tests are obtained on initial evaluation and periodically to assess for any changes. ALD occurrence remans high and without a public health effort will continue to increase in coming years.
………………………………………………………………,
TIPS procedure
https://youtu.be/O2u4_hF3234?si=E7v8Na1xUW8tekFp
Thank you for reviewing this post. Feedback or comments are welcome jeffk072261@gmail.com For education and information purposes only. This post should not be considered medical or professional advice. Data and images obtained from sources available in the World Wide Web. References used in preparation of this post are listed below.
References
Pathogenesis of liver cirrhosis
Wen-Ce Zhou, Quan-Bao Zhang, Liang Qiao
World J Gastroenterol 2014 June 21; 20(23): 7312-7324 ISSN 1007-9327 (print) ISSN 2219-2840 (online) © 2014 Baishideng Publishing Group Inc.
Treatment of Severe Alcoholic Hepatitis
Mark Thursz uand Timothy R. Morgan
1Division of Digestive Diseases, Imperial College, St Mary’s Hospital Campus, London, United Kingdom
2Gastroenterology Services, VA Long Beach
Gastroenterology . 2016 June ; 150(8): 1823–1834. doi:10.1053/j.gastro.2016.02.074.
……………………………………………………….
Hepatocyte pyroptosis and release of inflammasome particles induce stellate cell activation and liver fibrosis
Author links open overlay panel
Volume 74, Issue 1, January 2021, Pages 156-167
Autophagy Dysregulation in Metabolic Associated Fatty Liver Disease: A New Therapeutic Target
by Chun-Liang Chen 1
and Yu-Cheng Lin 1,2,*
Department of Pediatrics, Far Eastern Memorial Hospital, New Taipei City 220, Taiwan
School of Medicine, National Yang Ming Chiao Tung University, Taipei City 112, Taiwan
Int. J. Mol. Sci. 2022, 23(17), 10055; https://doi.org/10.3390/ijms231710055
……………………………………………………………
STING mediates hepatocyte pyroptosis in liver fibrosis by Epigenetically activating the NLRP3 inflammasome
Author links open overlay panel
Yang Xiao a b 1, Chong Zhao a b 1, Yang Tai a b 1, Bei Li c 1, Tian Lan a b, Enjiang Lai a b, Wenting Dai a b,
Volume 62, June 2023, 102691
Pathophysiology and Management of Alcoholic Liver Disease: Update 2016
Felix Stickel1, Christian Datz2, Jochen Hampe3, and Ramon Bataller4
1Department of Gastroenterology and Hepatology, University Hospital Zurich, Zurich, Switzerland,
Gut and Liver, Vol. 11, No. 2, March 2017, pp. 173-188
, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5347641/pdf/gnl-11-173.pdf
……………………………………………………………
Genetic and epigenetic disease modifiers: non-alcoholic fatty liver
disease (NAFLD) and alcoholic liver disease (ALD)
Narendra Singh Choudhary1, Ajay Duseja2
1Institute of Liver Transplantation and Regenerative Medicine, Medanta, The Medicity, Gurgaon, Delhi (NCR), India; 2Department of Hepatology,
Postgraduate Institute of Medical Education and Research, Chandigarh, India
Transl Gastroenterol Hepatol 2021;6:2 | http://dx.doi.org/10.21037/tgh.2019.09.06
Francesca Virginia Bruschi, Matteo Tardelli, Thierry Claudel & Michael Trauner (2017) PNPLA3 expression and its impact on the liver: current perspectives, Hepatic Medicine: Evidence and Research, , 55-66, DOI: 10.2147/HMER.S125718
https://www.tandfonline.com/doi/pdf/10.2147/HMER.S125718
Video: Overview of Alcohol-Related Liver Disease-Merck Manual Professional Edition
………………………………………………………………………..
Association of Genetic Variation With Cirrhosis: A Multi-Trait Genome-Wide Association and Gene–Environment Interaction Study
Connor A. Emdin
Mary Haas Veeral Ajmera Rohit Loomba Sekar Kathiresan Amit V. Khera
Published:December 10, 2020DOI:https://doi.org/10.1053/j.gastro.2020.12.011
…………………………………………………………..
The Epidemiology of
Alcoholic Liver Disease
Robert E. Mann, Ph.D., Reginald G. Smart, Ph.D., and Richard Govoni, Ph.D.
……………………………………………………………….
………………………………………………………………
WJG 20th Anniversary Special Issues (10): Alcoholic Liver Disease
Diagnosis of alcoholic liver disease
Cara Torruellas, Samuel W French, Valentina Medici
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155359/pdf/WJG-20-11684.pdfh
PRACTICE GUIDANCE | Hepatology, Vol. 71, No. 1, 2020
Diagnosis and Treatment of
Alcohol-Associated Liver Diseases: 2019
Practice Guidance From the American
Association for the Study of Liver Diseases David W. Crabb,1 Gene Y. Im ,2 Gyongyi Szabo,3 Jessica L. Mellinger,4 and Michael R. Lucey5
https://aasldpubs.onlinelibrary.wiley.com/doi/pdfdirect/10.1002/hep.30866
…………………………………………………………….
ARTICLES| VOLUME 5, ISSUE 6, E316-E323, JUNE 2020
Projected prevalence and mortality associated with alcohol-related liver disease in the USA, 2019–40: a modelling study
Jovan Julien, MS Turgay Ayer, PhD Emily D Bethea, MD Elliot B Tapper, MD Jagpreet Chhatwal, PhD
Open AccessPublished:June, 2020DOI:https://doi.org/10.1016/S2468-2667(20)30062-1
Pathogenesis of alcoholic liver disease: Role of oxidative metabolism
Elisabetta Ceni, Tommaso Mello, Andrea Galli
World J Gastroenterol 2014 December 21; 20(47): 17756-17772 ISSN 1007-9327 (print) ISSN 2219-2840 (online) © 2014 Baishideng Publishing
……………………………………………………….
CYEP21 cytochrome system
……………………………………………………….
Pavlov CS, Casazza G, Nikolova D, Tsochatzis E, Burroughs AK, Ivashkin VT, Gluud C. Transient elastography for diagnosis of stages of hepatic fibrosis and cirrhosis in people with alcoholic liver disease. Cochrane Database of Systematic Reviews 2015, Issue 1. Art. No.: CD010542. DOI: 10.1002/14651858.CD010542.pub2. Accessed 18 June 2024.
………………”………………………………………..k
International Journal of Ultrasound Physics
Review Article
Basic Physics of Ultrasound Elastography
Maurizio Cè1,*, Natascha Claudia D’Amico2 and Michaela Cellina3
1Postgraduate School in Diagnostic and Interventional Radiology, University of Milan, Italy
2Data Scientist, IQVIA, Frankfurt, Hesse, Germany
3Department of Radiology, ASST Fatebenefratelli Sacco, Italy
*Corresponding author: Maurizio Cè, BA MD, Postgraduate School in Radiology, University of Milan, Via Festa del Pedono,
7, 20122, Milan, Italy
Received:November 14, 2022 Published: December 09, 2022
Clinical Studies & Medical Case Reports
………………………………………………………..
What is a pascal as a unit of pressure or stress?
…………………………………………………….
Is transient elastography a useful tool for screening liver disease?
Paolo Del Poggio, Silvia Colombo
,World J Gastroenterol 2009 March 28; 15(12): 1409-14
……………………………………………………….
Sheth, M., Riggs, M. & Patel, T. Utility of the Mayo End-Stage Liver Disease (MELD) score in assessing prognosis of patients with alcoholic hepatitis. BMC Gastroenterol 2, 2 (2002). https://doi.org/10.1186/1471-230X-2-2
https://link.springer.com/article/10.1186/1471-230X-2-2#citeas
…………………………………………………….
Long-term prognostic value of the FibroTest in patients with non-alcoholic fatty liver disease, compared to chronic hepatitis C, B, and alcoholic liver disease
Mona Munteanu, Raluca Pais, Valentina Peta, Olivier Deckmyn, Joseph Moussalli, Yen Ngo, Marika Rudler, Pascal Lebray, Frederic Charlotte, Vincent Thibault … See all authors
First published: 17 October 2018 https://doi.org/10.1111/apt.14990C
Alimentary Pharmacology & Therapeutics | Pharmacology Journal | Wiley Online Library
………………………………………………………..
Prognostic and diagnostic scoring models in acute alcohol- associated hepatitis: A review comparing the performance of different scoring systems
…………………………………………………….
Alcoholic Hepatitis: A Review
Nooshin Hosseini1, Julia Shor1, and Gyong
Alcohol and alcoholism 2019 54(4)
……………………………………………………….
Clinical applications of the Model for End-Stage Liver Disease (MELD) in hepatic medicine
Hepatic Medicine Evidence and Research 8 February 2013
…………………………………………………………
MELD score | Radiology Reference Article | Radiopaedia.org
…………………………………………………………….
MELD score as a predictor of mortality, length of hospital stay, and disease burden: A single-center retrospective study in 39,323 inpatients.
Roth JA Chrobak C , Schädelin S , Hug BL
Medicine, 01 Jun 2017, 96(24):e7155
https://doi.org/10.1097/md.0000000000007155 PMID: 28614247 PMCID: PMC5478332
https://europepmc.org/article/med/28614247
……………………………………………………………………
Gene signature-MELD score and alcohol relapse determine long-
term prognosis of patients with severe alcoholic hepatitis
Pierre Deltenre, Eric Trépo1, Naoto Fujiwara, Nicolas Goossens,
Liver Int . 2020 PMC 2021 March
………………………………………………………………..
Combination of Gene Expression Signature and Model for End-Stage Liver Disease Score Predicts Survival of Patients With Severe Alcoholic Hepatitis
Eric Trépo,1,2,* Nicolas Goossens,3,4,* Naoto Fujiwara,
Gastroenterology 2018;154:965–975
https://www.gastrojournal.org/article/S0016-5085%2817%2936367-9/pdf
………………………………………………………………..
DNA microarray
………………………………………………………………….
Alcohol Abstinence Improves Prognosis Across All Stages of Portal Hypertension in Alcohol-Related Cirrhosis
Benedikt Silvester Hofer 1 2 3, Benedikt S
Clinical Gastroenterology and Hepatology
Volume 21, Issue 9, August 2023, Pages 2308-2317.e7
https://www.sciencedirect.com/science/article/pii/S1542356522011132
……………………………………………………………….
Alcoholic liver disease confers a worse prognosis than HCV infection and non-alcoholic fatty liver disease among patients with cirrhosis: An observational study
Astrid Marot, Jean Henrion, Jean-François Knebel, Christophe Moreno, Pierre Deltenre
Published: October 27, 2017 https://doi.org/10.1371/journal.pone.0186715
……………………………………………………………..
Development and prognostic relevance of a histologic grading and staging system for alcohol-related liver disease
Carolin Lackner Rudolf E. Stauber Susan Davies Helmut Denk Hans Peter Dienes Viviane Gnemmi
Volume 75, Issue 4, October 2021, Pages 810-819
………………………………………………………..
………………………………………………………
Model for End Stage Liver Disease (MELD) Score: A Tool for Prognosis and Prediction of Mortality in Patients With Decompensated Liver Cirrhosis
Isioma Emenena 1 , Bright Emenena 2 , Anthony G. Kweki 3 , Henry O. Aiwuyo 4 , John O. Osarenkhoe 5 , Ugoeze N. Iloeje 6 , Nosakhare Ilerhunmwuwa 7 , Beatrice E. Torere 8 , Oluwasegun Akinti 4
……………………………………………….
Alcoholic liver disease: A current molecular and clinical
perspective☆
Koichiro Ohashia
, Michael Pimientaa,b, and Ekihiro Sekia,b,c,d,*
aDivision of Digestive and Liver Diseases, Department of Medicine, Cedars-Sinai Medical Center,
Los Angeles, CA, USA
bUniversity of California San Diego, School of Medicine, La Jolla, CA, USA
……………………………………………….,.,,,,,
THE ROLE OF GENETIC POLYMORPHISMS IN ALCOHOLIC LIVER DISEASE
FELIX STICKEL, CHRISTOPH H. ÖSTERREICHER
Alcohol and Alcoholism, Volume 41, Issue 3, May/June 2006, Pages 209–224, https://doi.org/10.1093/alcalc/agl011
………………………………………………………….
The Genetics of Alcohol Dependence and Alcohol-related
Liver Disease
Felix Stickel1*, Christophe Moreno2,3, Jochen Hampe4, Marsha Y. Morgan5
J HEPAT-S-16-01356
Jk/07/24
Jeffk072261@gmail.com


Leave a comment