Function & Applications
The previous post told the story of the discovery of the endocannabinoid system and introduction to its central components. This post takes a closer look at how this system functions and potential clinical applications.

As noted previously there are two known endocannabinoids, these are Anandamide (AEA) and 2-AG. They are fatty molecules and are synthesized locally within cells to meet demand.
There are two receptor types present. These are called CB1 and CB2. CB1 receptors are most common in the brain and CB2 is most common in immune and GI organs. Both types overlap and may be found in the same locations. Receptors are located on cell membranes. Both types of endocannabinoids (EC) can bind to either type of receptor.
Once the EC has docked to a receptor a chain of reactions occur resulting in a change in cell function. Both long and short term functional changes have been observed.

The EC system works by a unique mechanism known as retrograde signaling. In this pathway a neuron releases its neurotransmitter which is received by an adjacent neuron . The receiving neuron then releases an endocannabinoid which feeds back to the sending neuron. This results in inhibition and the cell stops or slows down activity.
To make things more complex receptors can be present on either excitatory Glutamate or inhibitory GABA neurons. Thus the end result can vary depending on local conditions.
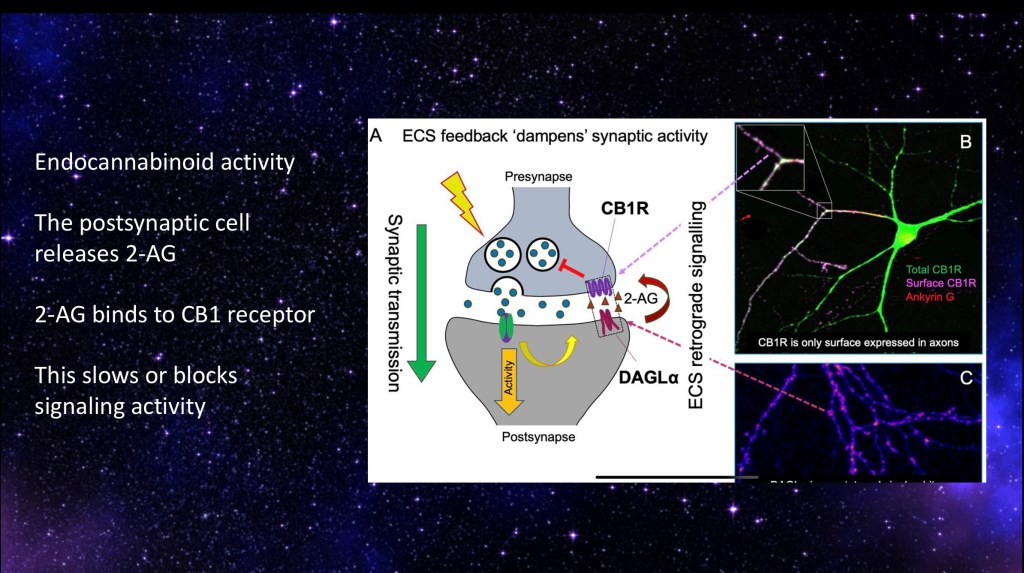
Another example illustrating how ECs work in the cell. A presynaptic neuron releases a neurotransmitter. This results in production of endocannabinoid 2-AG which feeds back, binding to a CB1 receptor. The result is inhibition of further activity from the presynaptic cell.
On the right are micrographs demonstrating fluorescent stained CB1 surface receptors on cell axons.

Glutamate (green=go) and GABA (red=stop) neurons with synaptic connections to the same cell. The strength of 2-AG endocannabinoid signal on one or the other will determine post synaptic activity.
Significant individual variation has been noted between males and females. Females tend to have higher baseline CB1 levels. Receptor levels and endocannabinoid levels also vary between individuals and throughout the day. The system is highly dynamic and responsive to internal and external factors.

Circled in red are four potential steps which could be targets for a designer agent to achieve a desired therapeutic outcome.
- Give a cannabinoid that activates CB1 or CB2 receptors (agonist)
- Give an agent that blocks cannabinoid receptor activity. (antagonist)
- Give an agent that affects endocannabinoid synthesis, increasing or decreasing EC supply.
- Give an agent that affects endocannabinoid degradation, either breaking it down faster or keeping it around longer.
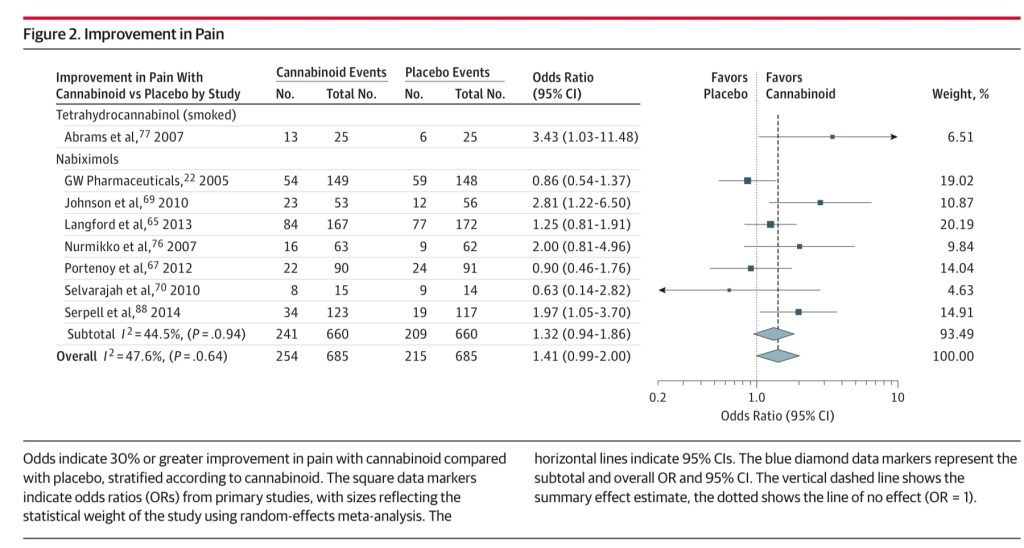
This clinical review looked at 79 published placebo controlled studies evaluating THC/CBD or synthetic cannabinols for a number of indications. Outcomes measured were analgesia, nausea/vomiting, weight loss due to HIV, depression, anxiety, muscle spasm, sleep disorder, psychosis, glaucoma or Tourette syndrome.
Of the studies reviewed significant positive outcome was found for only two conditions. There was moderate quality evidence for chronic pain relief and low evidence for improved nausea/vomiting secondary to chemotherapy.
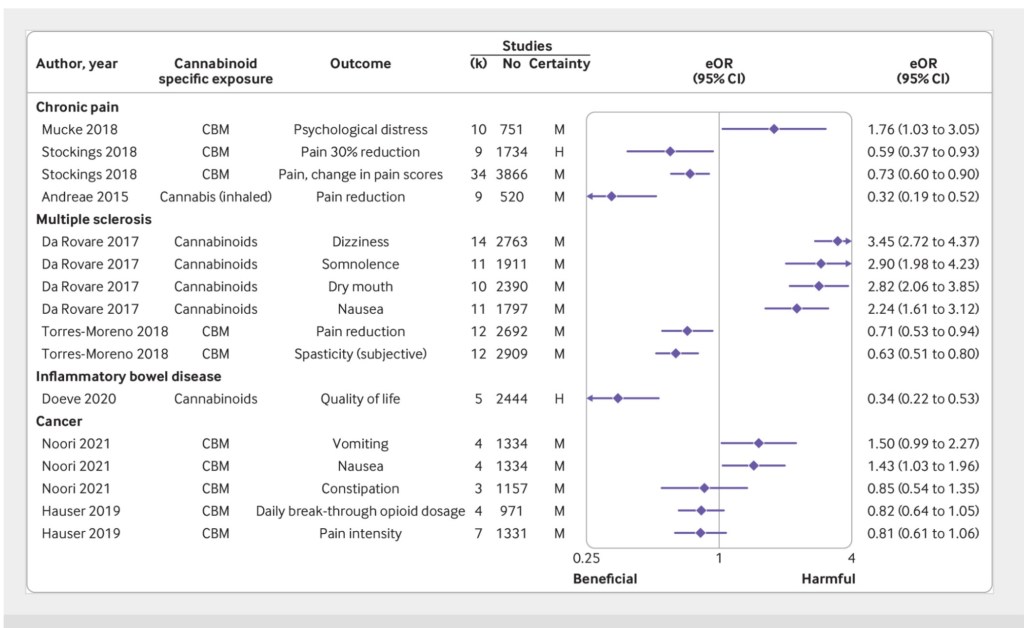
This meta-analysis recently published in the British Medical Journal in August 2023 looked at 101 published observational and interventional studies on the medical uses and effects of cannabis based medicines and smoked cannabis. Studies were included based on a number of quality measures.
Findings were similar to what has been previously noted. There was strong evidence for CBD preparations for childhood epilepsy. There was good evidence for benefit for chronic pain, MS, IBS, and cancer complications. Adverse effects from cannabis use included increased risks for psychosis and mental health risks, cognitive impairment, and traffic accidents. Researchers did note relative lack of high quality studies which they attributed to legal and social restrictions.

Rimonabant is a CB1 blocking agent. It was marketed as an anti obesity drug. It was never approved by the FDA however it was approved in the EU in 2006. The drug was later discontinued due to reported cases of psychosis. The agent has been used extensively in research largely in animal studies. It had been studied as a possible medication for treatment of substance use disorder. There is little current interest in further investigation due to significant adverse effects.
Dronabinol is an oral standardized THC based medication which was FDA approved in 1985 and is currently in use as an antiemetic in patients undergoing chemotherapy.
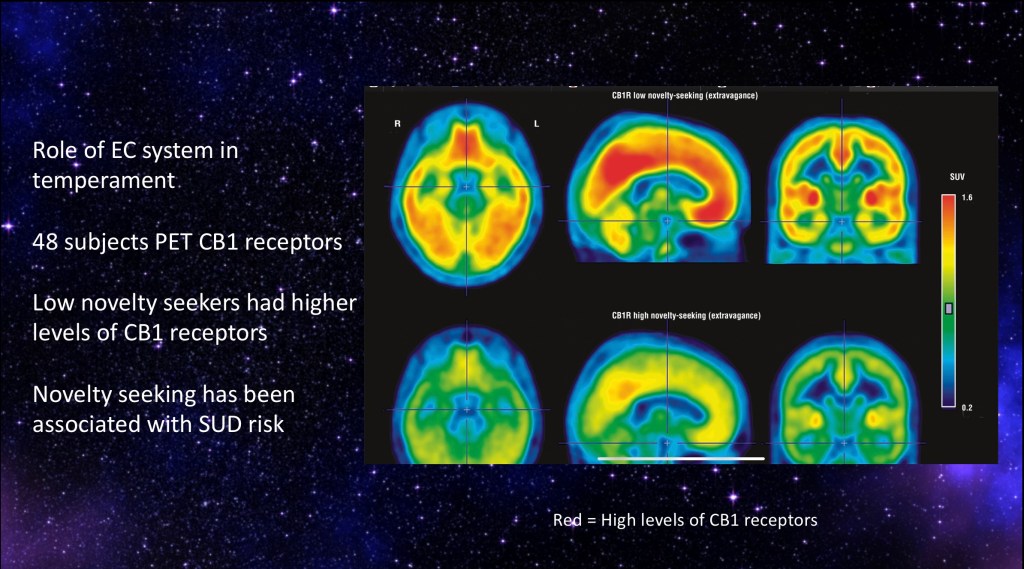
This study investigated CB1 receptor availability as it relates to the personality trait of novelty seeking. The 48 subjects completed psychometric testing along with PET using a CB1 receptor binding agent.
Imaging above demonstrates that high novelty seeking individuals had lower baseline CB1 levels. Novelty seeking has been associated with increased incidence of substance use disorder. It should be noted that personality traits are highly complex and the study only indicates a correlation.
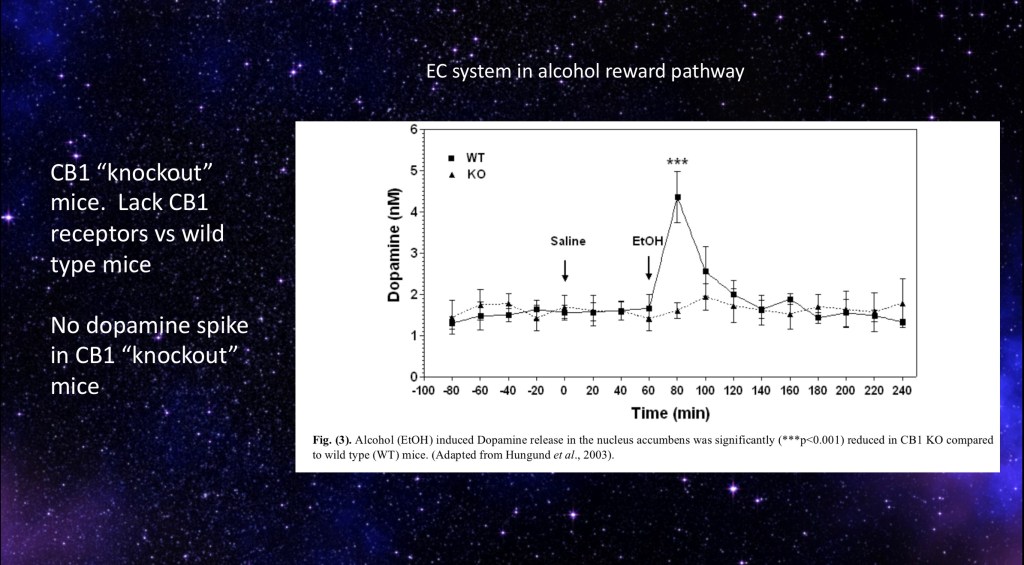
This study involved the use of CB1 “knockout mice”. These are mice which have had the gene for the receptor deleted. To breed knockout mice a DNA sequence is introduced rendering the gene inoperable. Several generations of -/- mice are bred to ensure an otherwise heterogeneous population.
Dopamine levels were measured by microdialysis before and after ethanol administration. Results are as above with no dopamine spike present in the CB1 negative mice.

Genetic mutations in the endocannabinoid system have been implicated to play a role in problematic drug/alcohol use. This study found a human DNA mutation in the gene coding for the enzyme FAAH. FAAH breaks down the endocannabinoid AEA in cells. A mutation of this gene results in higher endocannabinoid levels.
The study found that people with this mutation had a much higher chance of reported drug/alcohol related problems compared to controls.
This and other studies have demonstrated a definitive role for the cannabinoid system in acute and chronic effects of alcohol and other addictive substances.
Since the discovery of the endogenous system of cannabinoid molecules and receptors in the early 1990s there has been considerable research effort into understanding how it functions and how it can be harnessed to achieve therapeutic goals. This post has reviewed some of what has been learned about the components of this system.

^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^
Thank you for your consideration in reviewing this post.
For information and educational purposes only. No commercial or institutional interests. Data and images obtained from sources freely available on the World Wide Web. This post should not be considered medical or professional advice.
References
Nat Rev Dis Primers. ; 7(1): 16. doi:10.1038/s41572-021-00247-4.
Cannabis use and cannabis use Disorder
Jason P. Connor1,2,✉, Daniel Stjepanović1, Bernard Le Foll3,4, Eva Hoch5,6, Alan J. Budney7, Wayne D. Hall1,8
………………………………………..
Pharmacol Rev. 2006 September ; 58(3): 389–462.
The Endocannabinoid System as an Emerging Target of Pharmacotherapy
PÁL PACHER, SÁNDOR BÁTKAI, and GEORGE KUNOS
Laboratory of Physiologic Studies, National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health, Bethesda, Maryland
……………………………………………………
Relationship of Type 1 Cannabinoid Receptor Availability in the Human Brain to Novelty-Seeking Temperament
Koen Van Laere, MD, PhD, DrSc; Karolien Goffin, MD; Guy Bormans, PhD; et al
Cindy Casteels, MSc; Luc Mortelmans, MD, PhD, Ir; Jan de Hoon, MD, PhD, MSc; Igor Grachev, MD, PhD; Mathieu Vandenbulcke, MD, PhD; Guido Pieters, MD, PhD
Arch Gen Psychiatry. 2009;66(2):196-204
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/210206
……………………………………………………………
Involvement of the endocannabinoid
system in drug addiction
Rafael Maldonado, Olga Valverde and Fernando Berrendero
TRENDS in Neurosciences Vol.29 No.4 April 2006
…………………………………………….
Cannabinoids and the endocannabinoid system in reward processing and addiction: from mechanisms to interventions
R Spanagel
Trends in Neuroscience
Pages 241-250 | Published online: 01
https://www.tandfonline.com/doi/full/10.31887/DCNS.2020.22.3/rspanagel
……………………………………………………..
Cannabinoid Receptors and the Endocannabinoid System: Signaling and Function in the Central Nervous System
Faculty of Pharmaceutical Sciences, The University of British Columbia, Vancouver, BC V6T 1Z4, Canada
Int. J. Mol. Sci. 2018, 19(3), 833; https://doi.org/10.3390/ijms19030833
https://www.mdpi.com/1422-0067/19/3/833
………………………………………..
Hirvonen, J., Zanotti-Fregonara, P., Umhau, J. et al. Reduced cannabinoid CB1 receptor binding in alcohol dependence measured with positron emission tomography. Mol Psychiatry18, 916–921 (2013). https://doi.org/10.1038/mp.2012.100
https://www.nature.com/articles/mp2012100#article-info
………………………………………
Cannabinoids for Medical Use
A Systematic Review and Meta-analysis
Penny F. Whiting, PhD; Robert F. Wolff, MD; Sohan Deshpande, MSc; et Al
…………………………………………………
Alcohol Clin Exp Res. 2020 April ; 44(4): 790–805. doi:10.1111/acer.14306.
Interactions Between Alcohol and the Endocannabinoid System
George Kunos
From the Division of Clinical and Biological Research, National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health, Bethesda, Maryland, United States.
…………………………………………………
Distinct functions of endogenous cannabinoid system in alcohol abuse disorders
Balapal S. Basavarajappa et Al.
BJP Received: 22 January 2019 Revised: 11 June 2019 Accepted: 18 June 2019
https://bpspubs.onlinelibrary.wiley.com/doi/pdfdirect/10.1111/bph.14780……………………………………………….
Balancing risks and benefits of cannabis use: umbrella review of meta-analyses of randomised controlled trials and observational studies
BMJ 2023; 382 doi: https://doi.org/10.1136/bmj-2022-072348 (Published 30 August 2023)
Cite this as: BMJ 2023;382:e072348
https://www.bmj.com/content/382/bmj-2022-072348
…………………………………………………………………
Jk 9/23

Leave a comment